3. Arterial Thrombosis
 Definition
Definition
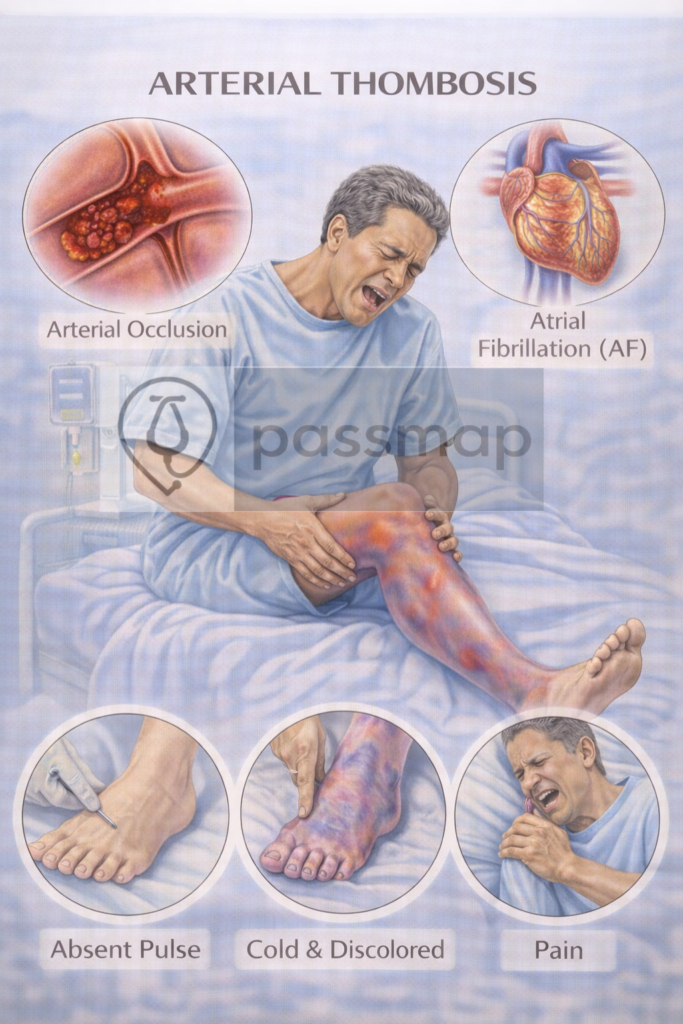
Arterial thrombosis is the formation of a blood clot in an artery, causing partial or complete obstruction of blood flow. It commonly leads to life-threatening events such as:
Myocardial infarction (MI) – Coronary artery thrombosis
Ischaemic stroke – Cerebral artery thrombosis
Acute limb ischaemia – Peripheral artery thrombosis
Pathophysiology
Arterial clots form primarily due to ruptured atherosclerotic plaques in high-flow vessels, leading to platelet-rich (“white”) thrombi.
Virchow’s triad in arterial thrombosis:
- Thrombosis (In-situ): Clot forms directly on a ruptured atherosclerotic plaque.
- Embolism (Traveling): Clot originates elsewhere (e.g., Atrial Fibrillation) and occludes a distal vessel.
- The “White Clot”: Driven by platelet aggregation; therefore, antiplatelets are the cornerstone of long-term management.
Risk Factors

Ageing
Tobacco use
Hypertension
Elevated lipids
Renal dysfunction
Obesity
Male sex
Atrial fibrillation (embolic risk)
🩺Clinical Features: The 6 P’s of Acute Limb Ischaemia
For the peripheral manifestation, you must know these in order:
Pain (Sudden onset, severe)
Pallor
Pulselessness
Paraesthesia (Sign of nerve ischaemia—Urgent)
Paralysis (Sign of muscle necrosis—Critical)
Perishingly cold
 EXAM ANCHOR – ACUTE LIMB ISCHAEMIA
EXAM ANCHOR – ACUTE LIMB ISCHAEMIA
PARA focuses heavily on the 6 P’s and the urgency of surgical referral.
The 6 P’s: Pain, Pallor, Pulselessness, Paraesthesia, Paralysis, Perishingly cold.
Threatened Limb: Paraesthesia and Paralysis are late signs indicating the limb is at risk of permanent necrosis.
Immediate Step: IV Unfractionated Heparin (UFH) bolus + Urgent Vascular Review.
Note: UFH is preferred over LMWH because it is quickly reversible with Protamine if emergency surgery is required.
📌 PARA commonly asks:
“A patient with AF has a cold, pulseless leg. What is the most appropriate immediate pharmacological step?”
Rutherford Classification for Acute Limb Ischaemia (ALI)
In exams, this classification helps you decide the “Best Next Step” based on the severity of the 6 P’s (specifically sensation and muscle power).
| Stage | Category | Clinical Features | Management |
| I | Viable | No sensory/motor loss. Capillary refill intact. Audible arterial Doppler signals. | Non-urgent; urgent imaging (CT Angio) and heparin. |
| IIa | Marginally Threatened | Minimal sensory loss (toes). No motor loss. Often inaudible arterial Doppler. | Urgent revascularisation needed. |
| IIb | Immediately Threatened | Sensory loss (beyond toes) + Motor loss (weakness). Inaudible arterial Doppler. | Emergency surgical intervention (Embolectomy/Bypass). |
| III | Irreversible | Complete anaesthesia + Paralysis (Rigor). All Doppler signals absent. Skin mottling. | Amputation (Revascularisation may cause reperfusion injury/death). |
Management

Aspirin (antiplatelet)
Clopidogrel or dual antiplatelet therapy (DAPT)
Long-term: Switch to Clopidogrel 75mg daily.
The Trap: Do not start Clopidogrel immediately in the acute phase; Aspirin is the priority for the first two weeks.
Thrombolysis (e.g. alteplase) – for stroke if within time window
Fibrinolysis (in STEMI or major embolism, if PCI not available)
Angioplasty / PCI or stenting (urgent)
Statin initiation
Treat underlying cause (e.g. hypertension, diabetes)
 EXAM ANCHOR – ACUTE LIMB ISCHAEMIA
EXAM ANCHOR – ACUTE LIMB ISCHAEMIA
PARA focuses on the “Urgent Referral” aspect.
Investigation: Handheld Doppler (if pulses not palpable). If Doppler signals are absent, it is a surgical emergency.
Immediate Management: IV Unfractionated Heparin (to prevent clot propagation).
Analgesia and IV fluids.
Urgent Vascular Review for reperfusion (Embolectomy vs. Bypass).
📌 PARA commonly asks:
“A patient has a cold, pulseless leg with loss of sensation. What is the most appropriate immediate pharmacological step?”
🔎 Key PARA Exam Traps
💡 Pulselessness: If a pulse is absent, the next step is Handheld Doppler, not immediate CT.
💡 AF Source: If the source of the arterial clot is Atrial Fibrillation, the patient must be on a DOAC long-term, not just Clopidogrel.
💡 Statins: For all arterial thrombosis, the dose is Atorvastatin 80mg (High-intensity), regardless of initial cholesterol levels.
💡 The 300mg Rule: For Ischaemic Stroke, Aspirin 300mg is given for 2 weeks before switching to Clopidogrel.
⚠️ Complications
Myocardial infarction
Stroke
Critical limb ischaemia → amputation
Death
📅 Last updated in line with:
NICE NG185 (ACS – 2025/26 Consolidated Update): Optimized antiplatelet choices and the unified “Invasive-First” framework.
NICE NG128 (Stroke/TIA – 2025 Update): Focusing on Tenecteplase as a first-line alternative to Alteplase and the 24-hour thrombectomy window.
NICE NG106 (PAD/Arterial Thrombosis – 2026 Review): Emphasizing Rapid Vascular Review for acute limb ischemia and the “300mg Aspirin for 2 weeks” rule for ischemic events.
PARA/MLA-aligned: Fully reviewed February 2026 for current Physician Associate and Medical Licensing Assessment blueprints.
🔒 PASSMAP Assurance: All content is peer-reviewed, NICE-compliant, and exam-optimized for the GMC Medical Licensing Assessment (MLA) and PA National Exam (PARA).
Educational platform. Not medical advice.
