7. Pleural Effusion
 Definition
Definition
A pleural effusion is the abnormal accumulation of fluid within the pleural space. It may be transudative (e.g. heart failure) or exudative (e.g. malignancy, infection).
🎯 EXAM ANCHOR – CORE CONCEPT
Pleural effusion = fluid accumulation in the pleural space
Classified as transudate or exudate
Cause determines management
📌 PARA commonly asks:
What is a pleural effusion?
🔬 Pathophysiology
🧠 Mnemonic: FLUID
Filtration imbalance (↑hydrostatic or ↓oncotic pressure → transudate)
Leaky pleura (↑permeability due to inflammation → exudate)
Unresolved infection or malignancy
Impaired lymphatic drainage
Disruption of pleural membrane or vessels
📋 Causes
🧠 Mnemonic: HEART PLUMP
Transudates:
Heart failure (most common)
End-stage renal disease (nephrotic syndrome)
Albumin low (cirrhosis, malnutrition)
Renal failure (fluid overload)
Thyroid (myxoedema)
Exudates:
Pneumonia (parapneumonic effusion)
Lung cancer
Unknown malignancy
Mesothelioma
Pulmonary embolism
🎯 EXAM ANCHOR – COMMON CAUSES (PARA)
Heart failure = most common cause overall
Malignancy = common cause of unilateral exudative effusion
Parapneumonic effusion common with infection
📌 PARA commonly asks:
What is the most common cause of pleural effusion?
 Clinical Features
Clinical Features
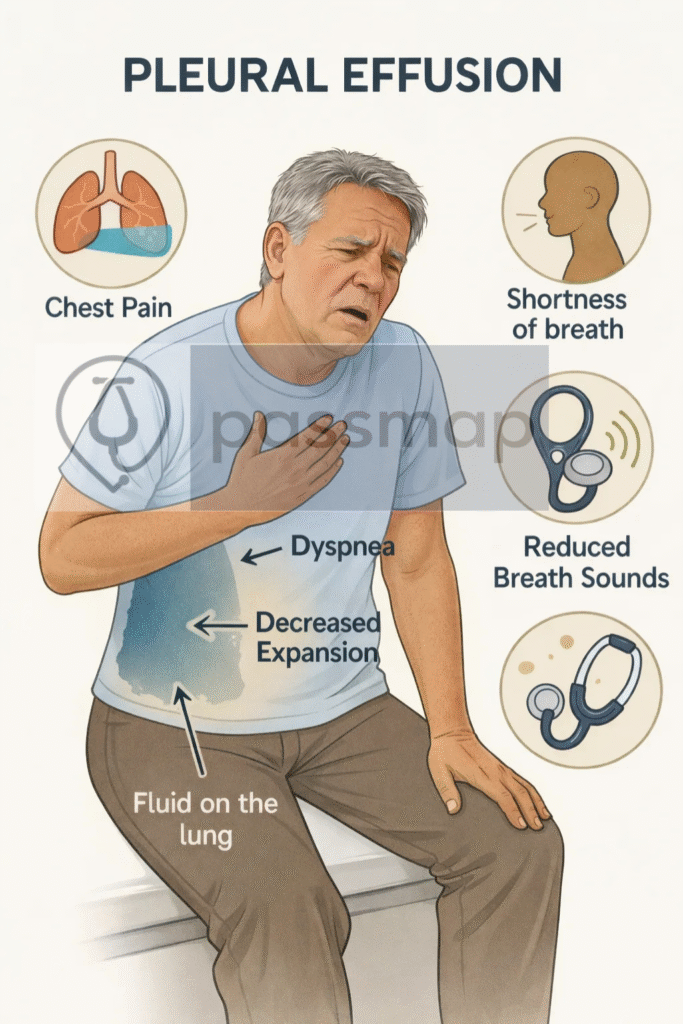
🧠 Mnemonic: SOB CHEST
Shortness of breath (especially on exertion)
Orthopnoea (if large effusion)
Breath sounds reduced
Chest pain (pleuritic)
Heavy feeling on affected side
Egophony above the fluid
Stony dull percussion
Trickling cough (dry, irritating)
🩺 Physical Examination Findings
Cachexia, pallor, lymphadenopathy
Finger clubbing
Crackles/bronchial breathing
Spinal tenderness (if Pott’s disease)
Signs of effusion or consolidation
🎯 EXAM ANCHOR – CLINICAL SIGNS
Reduced breath sounds
Stony dull percussion
Reduced chest expansion
Egophony above effusion
📌 PARA commonly asks:
What percussion note is expected in pleural effusion?
🔍 Investigations
🧠 Mnemonic: PLEURA
PA & lateral CXR – blunting of costophrenic angle ± meniscus sign
- Lung ultrasound – bedside confirmation (gold standard for guiding tap)
🎯 EXAM ANCHOR – IMAGING (PARA)
CXR shows blunted costophrenic angle
Ultrasound is best to confirm and guide aspiration
Small effusions may be missed on erect CXR
📌 PARA commonly asks:
What is the best investigation to confirm and guide pleural aspiration?
- Echo – rule out cardiac cause if transudate
Urgent aspiration if new unilateral effusion
Remember Light’s Criteria to differentiate
Analysis of pleural fluid:
Protein
LDH
pH
Cytology
Gram stain & culture
Acid-fast bacilli (TB)
🎯 EXAM ANCHOR – PLEURAL FLUID ANALYSIS
Send for protein, LDH, pH, cytology, culture
Low pH suggests infection or malignancy
Cytology may detect malignancy
📌 PARA commonly asks:
Which tests should pleural fluid be sent for?
Light’s Criteria Table – Differentiate Exudate vs Transudate
| Test Parameter | Exudate if ANY of the following is true: |
|---|---|
| Pleural fluid protein / Serum protein | > 0.5 |
| Pleural fluid LDH / Serum LDH | > 0.6 |
| Pleural fluid LDH | > ⅔ of upper limit of normal (ULN) serum LDH |
🔑 If any of these criteria are met → it’s an exudate.
🎯 EXAM ANCHOR – TRANSUDATE vs EXUDATE
Transudate: systemic cause (e.g. heart failure)
Exudate: local pathology (e.g. malignancy, infection, TB)
Differentiated using Light’s criteria
📌 PARA commonly asks:
Which investigation differentiates transudative from exudative pleural effusions?
🧾 Management
🧠 Mnemonic: DRAIN FLUID
Determine underlying cause
Radiology-guided thoracentesis if diagnostic
Antibiotics if parapneumonic
Intercostal drain if empyema / large infected
NSAIDs for pleuritic pain
🎯 EXAM ANCHOR – EMPYEMA
Empyema = infected pleural fluid
Requires intercostal chest drain
Repeated aspiration alone is insufficient
📌 PARA commonly asks:
What is the definitive management of empyema?
Follow-up imaging
Long-term drain or pleurodesis if malignant
Ultrasound to guide any further drainage
Investigate recurrent effusions
Discuss with respiratory if unclear
🎯 EXAM ANCHOR – ASPIRATION INDICATION
New unilateral pleural effusion should be aspirated
Exception: clear bilateral transudate responding to diuretics
Send fluid for full analysis
📌 PARA commonly asks:
When should a pleural effusion be aspirated?
⚠️ Complications
Empyema
Fibrosis/trapped lung
Sepsis
Pneumothorax (iatrogenic)
Re-expansion pulmonary oedema (rare but fatal)
🧐 Differentials
🧠 Mnemonic: POT HAIL
Pneumonia
Oedema (cardiogenic)
TB
Haemothorax
Asbestos exposure (mesothelioma)
Infarction (PE)
Lung malignancy
📌 PARA Revision Tips
Always confirm diagnosis and safety of aspiration with USS
Light’s Criteria is essential exam knowledge
Pleural tap = send for protein, LDH, pH, cytology, culture
Recurrent = think malignancy or TB
Consider chest drain if >1/2 hemithorax or infected
🎯 EXAM ANCHOR – RECURRENT EFFUSION (PARA)
Think malignancy or TB
May require pleurodesis or indwelling drain
MDT input required
📌 PARA commonly asks:
What should be suspected in recurrent pleural effusions?
🔎 Key PARA Exam Traps
💡 Dullness to percussion + reduced breath sounds = pleural effusion (not consolidation)
💡 CXR shows blunted costophrenic angles: Small effusions may be missed on erect CXR
💡 Ultrasound is the best test to confirm and guide aspiration
💡 Always aspirate a new unilateral pleural effusion: Unless clear cause (e.g. heart failure responding to diuretics)
💡 Light’s criteria differentiate transudate vs exudate: Exudate → malignancy, infection, PE, TB
💡 Heart failure causes bilateral transudative effusions: Asymmetrical or unilateral → think alternative cause
💡 Malignancy = common cause of unilateral exudative effusion
💡 Pleural effusion with fever and raised CRP → consider parapneumonic effusion or empyema
💡 Empyema requires chest drain: Repeated aspiration alone is insufficient
💡 Pleural effusion can mask underlying lung cancer: Always investigate the cause, not just drain
🔎 Last updated in line with NICE NG12 (2021) + BTS Guidelines (2023)
- PARA-aligned, reviewed February 2026
🔒 PASSMAP ensures all content is NICE-aligned and reviewed for Physician Associate Registration Assessment (PARA) success.
