2. Bronchiectasis
 Definition
Definition
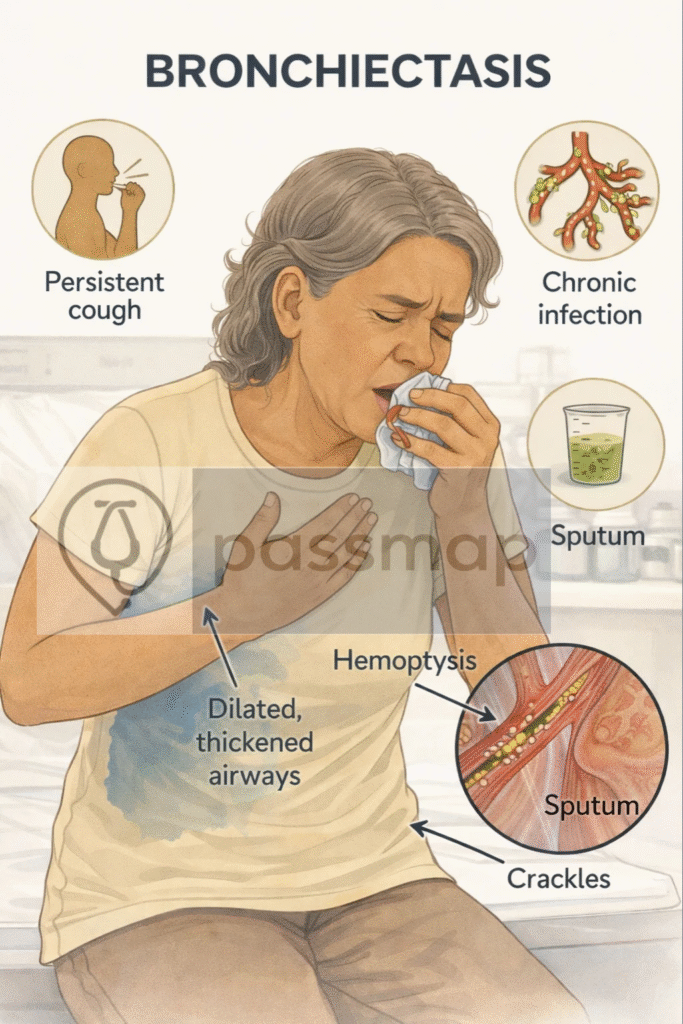
Bronchiectasis is an irreversible abnormal dilatation of the bronchi due to chronic infection and inflammation, resulting in impaired mucus clearance and persistent cough with sputum production.
🎯 EXAM ANCHOR – CORE CONCEPT (PARA)
- Bronchiectasis = irreversible bronchial dilatation
- Driven by chronic infection and inflammation
- Hallmark symptom = persistent productive cough
📌 PARA commonly asks:
A patient has irreversible airflow obstruction with daily productive cough and recurrent chest infections. What underlying structural abnormality explains this?
💡 PARA Differentiation Tip
COPD → irreversible airflow obstruction due to smoking-related airway/alveolar damage
Bronchiectasis → irreversible airflow obstruction due to structural airway dilatation + sputum
🧠 PARA Memory Trigger
“Wet lungs every day” → think bronchiectasis, not COPD or asthma
 Pathophysiology
Pathophysiology

Chronic infection →
Yielding inflammation
Ciliary damage
Loss of airway tone
Expansion of bronchi (permanent dilatation)
→ Leads to mucus stasis, colonisation, and recurrent infections.
📋 Causes
🧠 Mnemonic: ABCD SHIRT
Abnormal cilia (e.g. Kartagener’s, PCD)
Bronchial obstruction (tumour, foreign body)
Cystic Fibrosis
Deficiency (immune – IgA, IgG)
Systemic disease (RA, IBD, Sjogren’s)
Hypersensitivity (ABPA – allergic bronchopulmonary aspergillosis)
Infection (childhood measles, TB, pertussis)
Reflux/aspiration
Tuberculosis or other granulomatous infection
 Clinical Features
Clinical Features

-
Chronic productive cough
-
Overproduction of sputum (purulent, foul-smelling)
-
Up to 2+ exacerbations per year
-
Green/yellow mucus plugs
-
Haemoptysis (mild to massive)
-
Shortness of breath
-
Pleuritic chest pain
-
Infections recurrent
-
Tiredness (systemic symptoms)
🩺Physical Examination Findings
Bilateral coarse crackles ± wheeze
Clubbing
Signs of underlying cause (e.g. nasal polyps in CF, rash in vasculitis)
🔬 Investigation Ladder for Bronchiectasis
1️⃣ First-line Investigations (Initial Assessment)
| Test | Why / Exam Notes |
|---|---|
| CXR | May be normal; tram-track lines, ring shadows |
| Spirometry | Obstructive pattern (↓FEV₁, ↓FEV₁/FVC, little/no reversibility). Helps distinguish from asthma. |
| Sputum culture | Essential before antibiotics. Common bugs: H. influenzae, Pseudomonas, Staph aureus. |
🎯 EXAM ANCHOR 2 – ASTHMA / COPD DIFFERENTIATION
Asthma → reversible obstruction
Bronchiectasis → obstructive pattern with little/no reversibility
Chronic productive cough is key discriminator
📌 PARA commonly asks:
Which feature best differentiates bronchiectasis from asthma?
2️⃣ Second-line (Diagnostic Confirmation)
| Test | Why / Exam Notes |
|---|---|
| High-resolution CT (HRCT) | Gold standard |
| Tram-track sign | |
| Signet-ring sign (Internal bronchial diameter > its accompanying pulmonary artery.) | |
| Cystic dilatation |
 EXAM ANCHOR 3 – DIAGNOSIS (GOLD STANDARD)
EXAM ANCHOR 3 – DIAGNOSIS (GOLD STANDARD)
High-resolution CT (HRCT) = diagnostic gold standard
Key CT signs:
Tram-track sign
Signet-ring sign
Cystic bronchial dilatation
CXR may be normal and does not exclude bronchiectasis

Which investigation confirms bronchiectasis?
3️⃣ Third Line (Identify Underlying Cause)
| Test | Purpose |
|---|---|
| Immunoglobulins (IgA, IgG, IgM) | Detect immune deficiency. |
| Sweat test ± CFTR genetics | Rule out Cystic Fibrosis in young/adult-onset cases. |
| Aspergillus IgE / precipitins | Diagnose Allergic Bronchopulmonary Aspergillosis (ABPA) |
| Autoimmune screen (ANCA, RF) | If vasculitis/systemic disease suspected (e.g. GPA, RA, IBD). |
| HIV | If immunosuppression suspected. |
4️⃣ Targeted / Specialist Investigations
| Test | Indication |
|---|---|
| Bronchoscopy | Focal disease → exclude obstruction |
| Baseline bloods | Safety for long-term therapy |
5️⃣ Advanced / Specialist Care
| Intervention | Indication |
|---|---|
| Surgical resection | Localised severe disease |
| Lung transplant | End-stage disease |
💊 Management Ladder for Bronchiectasis
1️⃣ First-line (all patients)
| Intervention | Key Notes |
|---|---|
| Airway clearance physiotherapy | Chest physio + postural drainage = cornerstone of management. Daily routine. |
| Smoking cessation + vaccinations | Flu + pneumococcal essential. |
| Treat underlying cause | e.g. stop aspiration, treat immune deficiency, ABPA, CF. |
 EXAM ANCHOR 4 – FIRST-LINE MANAGEMENT LONG TERM MANAGEMENT
EXAM ANCHOR 4 – FIRST-LINE MANAGEMENT LONG TERM MANAGEMENT
First-line management includes Active Cycle of Breathing Techniques (ACBT) and checking/supplementing Vitamin D levels.
Antibiotics alone are not sufficient long-term management
Vaccinations + smoking cessation are mandatory supportive care

Most important long-term management strategy in bronchiectasis?

2️⃣ During Exacerbation
| Intervention | Key Notes |
|---|---|
| 14-day antibiotics (oral, guided by sputum culture) | Empirical if no result: amoxicillin (or doxycycline/clarithromycin if penicillin-allergic). Pseudomonas → ciprofloxacin. |
| Sputum culture at each exacerbation | Guides therapy + resistance monitoring. |
 EXAM ANCHOR 5 – EXACERBATIONS
EXAM ANCHOR 5 – EXACERBATIONS
Always send sputum culture before antibiotics
Treat exacerbations with 14-day antibiotics
If Pseudomonas aeruginosa is isolated for the first-time, NICE recommends eradication therapy (specialist-led) rather than standard symptom management.

Best next step in an acute exacerbation?
3️⃣ Long-term / frequent exacerbators
| Intervention | Key Notes |
|---|---|
| Long-term macrolides (azithromycin 3x/week) | If ≥3 exacerbations/year. Reduces exacerbation frequency. |
| Inhaled antibiotics (colistin, tobramycin) | For chronic Pseudomonas colonisation. Specialist-led. |
 EXAM ANCHOR 6 – FREQUENT EXACERBATORS
EXAM ANCHOR 6 – FREQUENT EXACERBATORS
≥3 exacerbations/year → consider long-term macrolide
Before starting long-term macrolides (Azithromycin), you must perform:
Sputum culture for NTM (Non-Tuberculous Mycobacteria) to prevent resistance.
Baseline ECG to check the QTc interval (Macrolides can prolong QTc).
Chronic Pseudomonas colonisation → inhaled antibiotics
Specialist supervision required

Indication for long-term antibiotics in bronchiectasis?
4️⃣ Adjunctive therapy
| Intervention | Key Notes |
|---|---|
| Mucolytics (e.g. carbocisteine) | May help sputum clearance. |
| Bronchodilators | If asthma/COPD overlap or reversible obstruction. |
5️⃣ Specialist referral / advanced care
| Intervention | Indication |
|---|---|
| Surgical resection (lobectomy) | Rare – for localised, severe, resistant disease. |
| Lung transplant | End-stage bronchiectasis with severe respiratory failure. |
⚠️ Complications
Respiratory failure
Massive haemoptysis
Pseudomonas colonisation
Pulmonary hypertension
Cor pulmonale
ABPA (allergic bronchopulmonary aspergillosis)
🎯 EXAM ANCHOR 7 – HAEMOPTYSIS (HIGH-RISK TRAP)
Mild haemoptysis = common
Massive haemoptysis = medical emergency
Requires urgent admission ± interventional radiology
📌 PARA commonly asks:
Which complication requires urgent escalation?
🧐Differentials

-
COPD
-
Haemoptysis from TB/lung cancer
-
Asthma
-
Pneumonia
-
Sinusitis/post-nasal drip
 Key PARA Exam Traps
Key PARA Exam Traps





🔎 Last updated in line with NICE NG117 – Bronchiectasis
Published: December 2018 • Last updated: February 2024
Last reviewed: February 2026
🔒 PASSMAP ensures all content is NICE-aligned and reviewed for Physician Associate Registration Assessment (PARA) success.
Educational platform. Not medical advice.
