5.1. Pneumonia (CAP & HAP)
📄 Definition
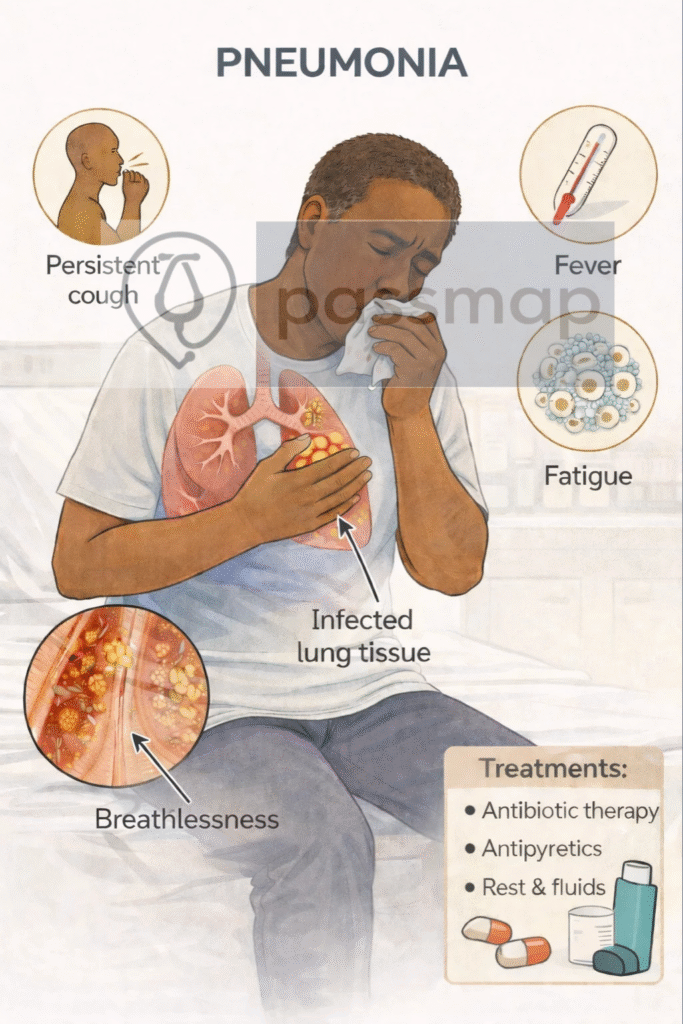
Pneumonia is an acute infection of the lung parenchyma causing consolidation, typically with cough, fever, and breathlessness.
🎯 EXAM ANCHOR – CORE CONCEPT (PARA)
Pneumonia = acute infection of lung parenchyma
Causes consolidation and impaired gas exchange
Presents with cough, fever, breathlessness
📌 PARA commonly asks:
What is pneumonia?
Types include:
CAP – Community-Acquired Pneumonia
HAP – Hospital-Acquired Pneumonia (onset ≥48 hours after admission)
🎯 EXAM ANCHOR – CAP vs HAP
CAP → onset in the community
HAP → onset ≥48 hours after hospital admission
Classification is based on timing, not organism
📌 PARA commonly asks:
How is hospital-acquired pneumonia defined?
Lobar or Unilateral
New infiltrates on imaging
Green/yellow sputum
Infection signs (fever, ↑CRP)
Neutrophilia
Fatigue
Elevated RR
Confusion (elderly)
Tachycardia
Inspiratory crackles
Overexertion breathlessness
Night sweats ± pleuritic pain
🎯 EXAM ANCHOR – ELDERLY PRESENTATION (PARA)
Elderly may present atypically
Confusion, falls, or functional decline may be the main feature
📌 PARA commonly asks:
How may pneumonia present differently in elderly patients?
Inhalation of microbes (e.g. Streptococcus pneumoniae)
→ alveolar inflammation
→ capillary leak + exudate
→ consolidation and impaired gas exchange
🛡️Causes (Aetiology)
Mnemonic: “B-FIT”
Bacterial – S. pneumoniae, H. influenzae, Legionella
Fungal – Aspergillosis, Pneumocystis jirovecii
Influenza viruses – Influenza A/B, RSV, COVID-19
Tuberculosis – M. tuberculosis (airborne)
Risk Factors
Mnemonic: SPLASH
Smoking
Pre-existing lung disease (COPD, asthma)
Low immunity (HIV, diabetes, cancer)
Age extremes (elderly, infants)
Steroids or immunosuppressants
Hospitalisation (for HAP)
 Clinical Features
Clinical Features
Mnemonic: COPS
Cough (productive ± blood-streaked)
Over 38°C fever
Pleuritic chest pain
Shortness of breath
Others: rigors, confusion (elderly), fatigue
Diagnosis
CXR = gold standard
FBC: neutrophilia
CRP, U&Es (for CRB65)
Blood cultures (if severe)
Sputum culture ± Legionella/pneumococcal urinary antigens
O₂ sats (ABG if <92%)
 EXAM ANCHOR – DIAGNOSIS
EXAM ANCHOR – DIAGNOSIS
Chest X-ray confirms pneumonia
Clinical features alone are insufficient
Normal early CXR does not exclude pneumonia

A patient presents with fever, cough, and pleuritic chest pain. Which investigation is required to confirm the diagnosis of pneumonia?
CXR Findings
Mnemonic: ABC of Consolidation
Air bronchograms
Bronchial wall thickening
Confluent opacity (lobar or patchy)
Lobar: homogeneous, sharp borders
Bronchopneumonia: multifocal, patchy
Aspiration: often lower zone, right lung
🎯 EXAM ANCHOR – ASPIRATION PNEUMONIA (PARA)
Occurs in dependent lung zones
Right lower lobe commonly affected
Risk factors: reduced consciousness, stroke, dysphagia
📌 PARA commonly asks:
Which lung zone is most commonly affected in aspiration pneumonia?
Severity Assessment – CRB65 Score (NICE)
Mnemonic: CRB65
Confusion (AMTS ≤8)
Respiratory rate ≥30
Blood pressure (SBP <90 or DBP ≤60)
65 years or older
| Score | Risk | Action |
|---|---|---|
| 0 | Low | Home treatment ± PO antibiotics |
| 1–2 | Moderate | Hospital referral |
| ≥3 | High | Urgent hospital admission ± ITU review |
🎯 EXAM ANCHOR – SEVERITY (CAP)
CRB-65 / CURB-65 assess severity, not diagnosis
Guides site of care decision
📌 PARA commonly asks:
Which score is used to assess severity in community-acquired pneumonia?
CRB65 is used in the community; CURB-65 is used in hospital settings where urea is available.
Management
➤ CAP
Mnemonic: CAP DOC
CRB65 (or CURB-65 if urea available) guides location of care
Amoxicillin 500 mg TDS 5 days (mild)
Penicillin allergy → doxycycline or clarithromycin
Dual therapy (amoxicillin + macrolide) if moderate/severe
Oxygen + fluids if needed
CXR repeat in 6 weeks if red flags (e.g. smoker, >50yrs)
➤ HAP
Within 5 days: cover Gram-positive + typicals
After 5 days: cover Gram-negative + resistant bugs
e.g. co-amoxiclav or piperacillin-tazobactam
🎯 EXAM ANCHOR – MANAGEMENT PRINCIPLE
CAP antibiotics guided by severity
HAP requires broader cover (Gram-negative ± resistant organisms)
Start antibiotics promptly after cultures (if indicated)
📌 PARA commonly asks:
Why does HAP require broader antibiotic coverage than CAP?
Monitoring & Follow-Up
O₂ sats, RR, temp, HR
Check CRP, WCC, and U&Es
Repeat CXR after 6 weeks if:
smoker
>50 yrs
slow resolution
lobar consolidation
🎯 EXAM ANCHOR – TREATMENT FAILURE
- No improvement at 48–72 hours → reassess
Consider:
Wrong diagnosis
Resistant organism
Complication (e.g. empyema)
📌 PARA commonly asks:
What should be considered if pneumonia does not improve after 48–72 hours of treatment?
Complications
Mnemonic: LIES
Lung abscess
Infection spread (empyema, sepsis)
Effusion (parapneumonic or empyema)
Scarred lung (fibrosis, bronchiectasis)
Differential Diagnoses
Mnemonic: PALM PECS
Pulmonary embolism
Asthma/COPD exacerbation
Lung cancer
Myocardial infarction
Pleural effusion
Eosinophilic pneumonia
COVID-19
Sarcoidosis
🔎 Key PARA Exam Traps
💡 CAP vs HAP is defined by timing, not organism: CAP = community onset; HAP = ≥48 hours after admission
💡 CURB-65 guides CAP severity, not diagnosis: Score ≥2 → consider admission; ≥3 → severe CAP
💡 CRP and WCC are non-specific: Use to support infection, not to identify pathogen
💡 CXR confirms pneumonia: Clinical features alone are insufficient
💡 Normal early CXR does not exclude pneumonia: Repeat imaging if high clinical suspicion
💡 Send sputum cultures before antibiotics in severe CAP or HAP
💡 HAP requires broader antibiotic cover: Think Gram-negative organisms and MRSA risk
💡 Failure to improve at 48–72 hours → reassess diagnosis, complications, or resistance
💡 Aspiration pneumonia → dependent lung zones; risk factors include stroke and reduced consciousness
💡 Elderly patients may present atypically: Confusion or falls may be the main feature
Last updated in line with NICE NG138 (October 2019)
- PARA-aligned, reviewed February 2026
PASSMAP ensures all content is NICE-aligned and exam-optimised for the Physician Associate Regulation Assessment (PARA).
Educational platform. Not medical advice.
