1. Asthma
 Definition
Definition
Chronic inflammatory airway disease with:
-
Reversible airflow obstruction
-
Airway hyperresponsiveness
-
Often linked to atopy and environmental triggers
Mnemonic: AIR
Airway inflammation
Intermittent symptoms
Reversible obstruction
🧬 Pathophysiology
-
Trigger (allergen, infection, exercise, cold air) → immune activation
-
Mast cells → histamine, leukotrienes → bronchial smooth muscle contraction
-
Eosinophils (IL-5 driven) → airway inflammation
-
Mucosal oedema + mucus hypersecretion → narrowed airways
🛡️ Risk Factors (Mnemonic: ASTHMIC)
Atopy (eczema, hay fever)
Smoking (active/passive)
Triggers (cold, dust, pets, pollen)
Household irritants (mould, damp)
Medications (NSAIDs, β-blockers)
Infections (esp. viral in childhood)
Childhood/family history
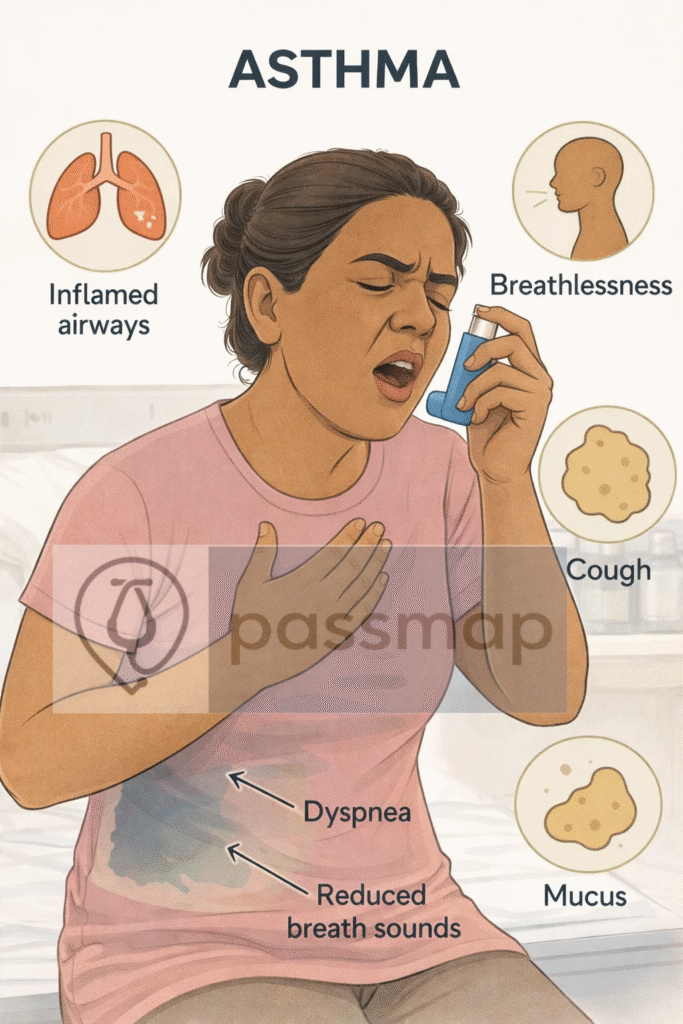
🤒 Symptoms (Mnemonic: WHACK)
Wheeze (expiratory, polyphonic)
Heavy chest (tightness)
At night/early morning (worse)
Cough (often dry, variable)
Keen trigger sensitivity (exercise, pets, dust, cold)
Symptoms are episodic and worse on exertion or allergen exposure.
🚩 Red Flags / Severe Features
Silent chest, exhaustion, confusion → impending respiratory failure
Life-threatening asthma: SpO₂ <92%, PEF <33%, silent chest, cyanosis, arrhythmia, hypotension
Near-fatal asthma: Raised PaCO₂ or need for mechanical ventilation
🔬 Investigations
| Test | Use | Exam Notes |
|---|---|---|
| Spirometry with reversibility | Obstructive pattern (FEV₁/FVC <70%) + ≥12% & ≥200 ml ↑ FEV₁ post-bronchodilator | Diagnostic gold standard |
| Peak flow monitoring | Variability >20% = diagnostic | Diurnal variation: morning dipping worse |
| FeNO | Raised in eosinophilic inflammation | NICE recommends in uncertain cases |
| Allergy testing | RAST/skin prick if atopy suspected | Not first-line |
| Bloods | May show eosinophilia | Rule out differentials |
| CXR | If atypical / to exclude pneumonia | Often normal in asthma |
 EXAM ANCHOR 1 – DIAGNOSIS
EXAM ANCHOR 1 – DIAGNOSIS
-
Asthma diagnosis requires evidence of variable airflow obstruction
-
Reversibility ≥12% AND ≥200 mL increase in FEV₁ post-bronchodilator = asthma
-
Normal spirometry does not exclude asthma (repeat or peak flow diary)

Which investigation confirms asthma?

🩻 CXR Findings (Mnemonic: THUMP)
Thickened bronchial walls
Hyperinflated lungs (flattened diaphragms)
Unusual findings suggest another cause
Mediastinal shift (if tension pneumothorax)
Pneumothorax / pneumomediastinum
🎯 EXAM ANCHOR 2 – ASTHMA vs COPD
Asthma = reversible obstruction
COPD = fixed/irreversible obstruction
Asthma often:
Younger onset
Atopy
Diurnal variability
📌 PARA commonly asks:
Which feature best differentiates asthma from COPD?
📊 Severity of Acute Asthma (BTS/NICE)
| Classification | Features |
|---|---|
| Moderate | PEFR 50–75%, speaks in full sentences |
| Severe | PEFR 33–50%, RR >25, HR >110, can’t finish sentences |
| Life-threatening | PEFR <33%, SpO₂ <92%, silent chest, cyanosis, confusion, hypotension |
🎯 EXAM ANCHOR 3 – ACUTE SEVERITY
PEF <33% = life-threatening asthma
Raised PaCO₂ = near-fatal asthma
Silent chest = impending respiratory failure
📌 PARA commonly asks:
Which feature indicates life-threatening asthma?
🎯 EXAM ANCHOR 3 – ACUTE SEVERITY
Life-Threatening “Normality”: A “normal” PaCO₂ (4.6–6.0 kPa) during an acute asthma attack is life-threatening.
It indicates respiratory muscle exhaustion — the patient can no longer hyperventilate to blow off CO₂.
A raised PaCO₂ signifies near-fatal asthma and impending ventilatory failure.
📌 PARA commonly asks:
A 24-year-old female presents to A&E with an acute asthma exacerbation. She is unable to complete sentences and has a respiratory rate of 30/min. An Arterial Blood Gas (ABG) is performed on room air. Which of the following ABG results is the MOST concerning sign of life-threatening exhaustion?
Stepwise Management (NICE 2022 Update)
Key Shift: MART Preferred
MART (Maintenance and Reliever Therapy) is now first-line for many adults and young people using:
Low-dose ICS-formoterol as both daily preventer and reliever
(e.g. Fostair, Symbicort)
🎯 EXAM ANCHOR 4 – FIRST-LINE PREVENTER (BIG PARA SHIFT)
Low-dose ICS-formoterol (MART) is preferred first-line in adults
SABA alone is no longer first-line if preventer indicated
Always review inhaler technique before stepping up
📌 PARA commonly asks:
What is the preferred first-line preventer strategy in adult asthma?
👉 Answer: MART (ICS-formoterol)
Mnemonic: SMART PLAN
- SABA no longer routinely used if on MART
- MART preferred for many (ICS-formoterol)
- Add-on therapy if uncontrolled: LTRA, ↑ICS
- Review inhaler technique and adherence
- Tailor plan to patient age and symptom pattern
- Personalised asthma action plan
- Low-dose ICS if not suitable for MART
- Adult vs child algorithms differ
- NICE stepwise diagram guides escalation
📋 Stepwise Treatment Ladder
🎯 EXAM ANCHOR 5 – WHEN TO START ICS
Start ICS if:
Symptoms ≥3 times/week
Night-time waking
Exacerbation requiring oral steroids
📌 PARA trap:
SABA-only treatment is not sufficient for frequent symptoms
| Step | Treatment | Notes |
|---|---|---|
| 1 | MART (low-dose ICS–formoterol) daily + PRN | Preferred adult first-line |
| 2 | Add LTRA (montelukast) before Increase ICS dose | Watch behavioural SE |
| 3 | Switch to alternative inhaler regimen or ↑ICS | Specialist review if uncontrolled |
| Children <5 | SABA trial → daily ICS if frequent | MART not licensed |
Offer a structured review to people with asthma at least annually.
More frequent reviews may be needed after treatment changes or exacerbations.
🎯 EXAM ANCHOR 6 – PAEDIATRIC TRAP
MART is NOT licensed in children <5
Different algorithms for children vs adults
📌 PARA commonly asks:
Which asthma management option is inappropriate in a 4-year-old?
🚨 Acute Asthma Management (Mnemonic: O SHIT ME)
Oxygen (aim SpO₂ 94–98%)
Salbutamol (neb or inhaler)
Hydrocortisone IV / Prednisolone PO
Ipratropium (neb, esp. in severe)
Theophylline (specialist input only)
Magnesium sulfate IV (for life-threatening cases)
Escalate care → HDU/ICU if deteriorating
🎯 EXAM ANCHOR 7 – ACUTE ASTHMA MANAGEMENT
Use oxygen to drive nebulisers in acute severe or life-threatening asthma
Add ipratropium in severe/life-threatening asthma
IV magnesium sulfate for life-threatening asthma
Early steroids reduce relapse and admission
📌 PARA commonly asks:
First-line management of acute severe asthma?
Monitoring & Review
Annual asthma review
Personalised Asthma Action Plan (PAAP)
Check inhaler technique and trigger control
Consider stepping down therapy if controlled for ≥3 months
⚠️ Complications
Mnemonic: RAMP
Respiratory failure
Air leaks – pneumothorax or pneumomediastinum
Mucus plugging
Persistent hypoxaemia
❓ Differential Diagnoses (Mnemonic: VACUUM)
Vocal cord dysfunction
Anaphylaxis
COPD
Upper airway obstruction
Undiagnosed cardiac disease (HF)
MSK chest pain
 Key PARA Exam Traps
Key PARA Exam Traps
Reversibility (≥12% AND ≥200 mL FEV₁) = asthma; irreversible airflow obstruction = COPD
Life-threatening asthma signs: silent chest, PEF <33%, SpO₂ <92%
Near-fatal asthma = raised PaCO₂ or need for ventilation
Always give oxygen with nebulised salbutamol (never air)
If LTRA ineffective, stop it and increase ICS or add LABA (do not continue ineffective LTRA – NICE)
Start ICS early if SABA ≥3 times/week
Montelukast → behavioural / neuropsychiatric side effects
ICS inhalers → rinse mouth to prevent oral candidiasis
MART regimen is for adults only
Cardioselective β-blockers (e.g. bisoprolol) may be used with caution — exam trap
Acute asthma + normal PaCO₂ (4.6–6.0 kPa) = respiratory muscle exhaustion → impending ventilatory failure
Montelukast + nightmares / suicidal ideation → stop immediately (MHRA)
Smoking reduces spirometry reliability; poor reversibility ≠ no asthma
📅 Last updated in line with:
NICE NG80 (Asthma: diagnosis, monitoring and chronic management) – Nov 2022
BTS/SIGN Asthma Guideline – 2019
PARA-aligned, reviewed February 2026
PASSMAP ensures all content is NICE-aligned and exam-optimised for the Physician Associate Regulation Assessment (PARA).
Educational platform. Not medical advice.
