📄 Definition
ACS = spectrum of conditions caused by acute myocardial ischaemia due to reduced coronary blood flow (usually a ruptured atherosclerotic plaque with thrombus).
Includes:
Unstable angina (UA) – ischaemic symptoms, no troponin rise, no ST elevation.
NSTEMI – troponin rise, no ST elevation.
STEMI – troponin rise, ST elevation or new LBBB.
 EXAM ANCHOR – NSTEMI vs. UNSTABLE ANGINA
EXAM ANCHOR – NSTEMI vs. UNSTABLE ANGINA
The distinction is based purely on biochemical evidence of myocardial necrosis:
NSTEMI: Ischaemic symptoms + Raised Troponin (I or T)
Unstable Angina: Ischaemic symptoms + Normal Troponin
Both typically show ST-depression, T-wave inversion, or a normal ECG.
📌 PARA commonly asks:
“A patient has chest pain at rest and ST-depression in V4-V6. Serial troponins are normal. What is the diagnosis?”
🛡️ Modifiable Risk Factors
Mnemonic: SHODDD
Smoking
HTN
Obesity
Diabetes
Dyslipidaemia (↑TC, ↑LDL, ↑TC:HDL)
Drinking (excess alcohol)
🔬 Pathophysiology
Plaque rupture/erosion → platelet adhesion + thrombus → partial or complete occlusion.
Complete occlusion → STEMI (transmural infarct).
Partial occlusion → NSTEMI/UA (subendocardial ischaemia)
↓ Blood flow → myocardial ischaemia ± infarction
🛡️ Non-Modifiable Risk Factors
Age ↑
Male sex
South Asian ethnicity
Family history: MI <55 in men, <65 in women
Personal history of MI, stroke, PVD
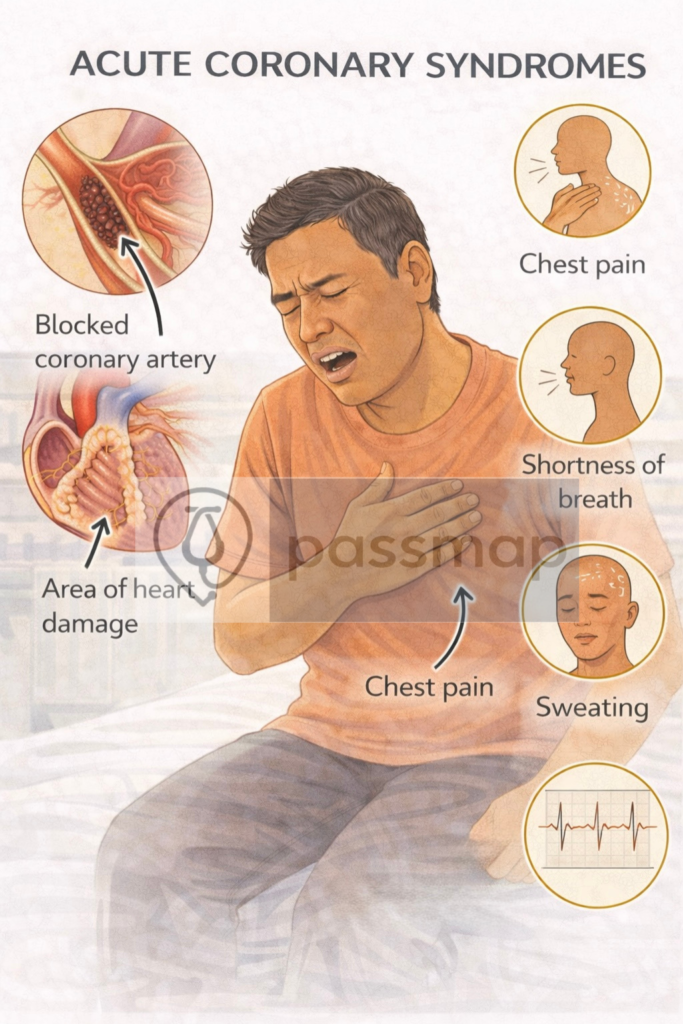
Symptoms – “Central CHEST Pain”
Crushing central chest pain
Heavy/tight (not sharp)
Exertional or at rest
SOB, Sweating, Nausea, Vomiting
Time >15 mins, not relieved by GTN
Radiation: Left arm, jaw, neck, back
Atypical in elderly, women or diabetic: may present with SOB alone or silent
🚩 Red Flags
Haemodynamic instability (SBP <90 mmHg).
Ongoing/refractory chest pain.
Life-threatening arrhythmia (VT/VF).
Acute heart failure or cardiogenic shock.
🔬 Investigations (Stepwise PARA Focus)
| Step | Test | Findings / Notes |
|---|---|---|
| 1️⃣ Bedside | ECG (12-lead within 10 min) | STEMI = ST elevation ≥2 mm in 2 adjacent chest leads or ≥1 mm in limb leads, or new LBBB. NSTEMI/UA = ST depression, T-wave inversion, or normal. Posterior MI – Reciprocal ST depression V1–V3 ± ST elevation in V7–V9 |
| Cardiac monitoring | Detect arrhythmias. | |
| 2️⃣ Labs | Troponin I/T | ↑ in NSTEMI/STEMI. Negative in UA. Serial (0 and 3 hrs). Causes of ↑troponin (HEART DIES): |
| FBC, U&E, LFT, CRP, glucose, lipids, coagulation | Risk stratification, comorbidities. | |
| 3️⃣ Imaging | CXR | Exclude other causes (dissection, pneumonia, HF). |
| Echo | LV function, complications (papillary rupture, free wall rupture). | |
| 4️⃣ Risk tools | GRACE score | Mortality risk → guides invasive strategy. |
 EXAM ANCHOR – STEMI CRITERIA
EXAM ANCHOR – STEMI CRITERIA
You must recognize these specific ECG findings to trigger the “120-minute PCI” clock:
ST-Elevation: ≥ 2 mm in two contiguous precordial leads (V1–V6) OR ≥ 1 mm in two contiguous limb leads.
New LBBB: A new Left Bundle Branch Block in the presence of chest pain is treated as a STEMI.
Posterior MI: ST-depression in V1-V3 with tall R-waves. (Look for ST-elevation in V7–V9).
📌 PARA commonly asks:
“A patient presents with chest pain and a new Left Bundle Branch Block. What is the next best step?”
Risk Stratification – GRACE Score
The GRACE (Global Registry of Acute Coronary Events) Score is the gold-standard tool recommended by NICE [NG185] for risk-stratifying patients with NSTEMI or Unstable Angina.
It calculates a percentage risk of death or recurrent MI within 6 months.
Mnemonic: GRACE → Guide Revascularisation After Clinical Evaluation
>6% risk → early PCI (<72h)
<3% risk → conservative ± conservative management without routine angiography
📌 PARA commonly asks:
“NSTEMI patient with GRACE score of 4%.” 👉 Angiography within 72 hours.
 Management – Stepwise
Management – Stepwise
A) Immediate (All Suspected ACS)
Initial stabilization follows the MONA (or ROMANCE) principles, emphasizing oxygen restriction:
Morphine: IV 5–10 mg + Antiemetic (Metoclopramide) if pain is severe.
Oxygen: Only if SpO₂ < 94% (or < 88% in COPD).
Nitrates: Sublingual GTN (or IV if persistent pain and SBP > 90 mmHg).
Aspirin: 300 mg loading dose (crushed or chewed).
📌 PARA commonly asks:
“A patient with central chest pain has oxygen saturations of 96%. What is the next step?”
B) STEMI (The Reperfusion Race)
The primary goal is rapid reperfusion based on the 120-minute window.
- Primary PCI: Offer if presenting within 12 hours of symptom onset and it can be delivered within 120 minutes of the time fibrinolysis could have been given.
- Prasugrel Choice: Offer prasugrel with aspirin if not already on an oral anticoagulant. Use clopidogrel instead if the patient is already taking an oral anticoagulant.
- Fibrinolysis: Offer if PCI is not possible within the 120-minute window. Perform an ECG 60–90 mins post-fibrinolysis; if ST-segment resolution is <50%, offer immediate angiography
 EXAM ANCHOR – STEMI REPERFUSION
EXAM ANCHOR – STEMI REPERFUSION
- Symptoms started within 12 hours
- AND PCI can be delivered within 120 minutes of the time fibrinolysis could have been given
Reperfusion (Primary PCI) is indicated if:
📌 PARA commonly asks:
A patient presents 4 hours after chest pain started. The nearest PCI center is 3 hours away. What is the most appropriate management?”
C) NSTEMI / Unstable Angina
Management is strictly risk-stratified using the GRACE score.
Acute Management Mnemonic: BATMAN
Base PCI decision on GRACE Score.
Aspirin: 300 mg loading.
Ticagrelor: 180 mg loading (or Clopidogrel 600 mg).
Morphine: IV for pain.
Antithrombin: Fondaparinux 2.5 mg SC (unless immediate PCI planned within 24h, unless immediate angiography is planned or high bleeding risk exists). Use dose-adjusted unfractionated heparin if creatinine is >265 µmol/L
Nitrates: Sublingual or IV.
Note: Avoid IV β-blockers if signs of heart failure or bradycardia.
 EXAM ANCHOR – INITIAL ANTITHROMBIN
EXAM ANCHOR – INITIAL ANTITHROMBIN
NICE recommends a specific agent as the first-line antithrombin for NSTEMI/UA:
First-line: Fondaparinux (unless immediate angiography is planned or high bleeding risk exists)
Renal Impairment: If Creatinine >265 µmol/L, use dose-adjusted Unfractionated Heparin (UFH)
📌 PARA commonly asks:
“A patient with NSTEMI has a creatinine of 310 µmol/L. Which antithrombin should be initiated?”
Invasive Strategy (Angiography) Timelines:
Immediate (< 2 hours): If haemodynamically unstable, refractory pain, or life-threatening arrhythmias.
Early (< 24 hours): If GRACE score > 140 or dynamic ST changes.
Standard (< 72 hours): If GRACE score > 3% (6-month mortality) or diabetic/renal impairment.
 EXAM ANCHOR – NSTEMI INVASIVE TIMELINE
EXAM ANCHOR – NSTEMI INVASIVE TIMELINE
The timeframe for coronary angiography is dictated by the GRACE Score (6-month mortality):
Intermediate/Higher Risk (>3%): Angiography within 72 hours
Low Risk (≤3%): Consider conservative management (no routine angiography)
📌 PARA commonly asks:
“An NSTEMI patient has a 6-month mortality risk of 4.5%. What is the appropriate timeframe for an invasive strategy?”
D) Secondary Prevention (The 6 As)
All patients should be discharged on these six elements to improve survival:
Aspirin: 75 mg once daily (lifelong).
Antiplatelet (2nd): Ticagrelor or Clopidogrel (usually for 12 months).
Atorvastatin: 80 mg daily (High-intensity statin).
ACE Inhibitor: (e.g., Ramipril) titrated to max dose.
Atenolol: (or other Beta-blocker, e.g., Bisoprolol).
Aldosterone Antagonist: (e.g., Eplerenone) if LVEF ≤ 40% and symptomatic HF.
 EXAM ANCHOR – SECONDARY PREVENTION TITRATION
EXAM ANCHOR – SECONDARY PREVENTION TITRATION
Evidence-based medication must be titrated to target doses:
ACE Inhibitors: Complete titration within 4 to 6 weeks of hospital discharge
Aldosterone Antagonist: Offer if LVEF is reduced; start 3 to 14 days after MI
Monitoring: Check U&Es and BP before starting ACEi and again after 1–2 weeks
📌 PARA commonly asks:
“When should the titration of an ACE inhibitor be completed following an MI?” 👉 Within 4–6 weeks of discharge
Dressler’s Syndrome
Mnemonic: F-PER
-
Fever
-
Pleuritic chest pain
-
Effusion (pericardial)
-
Raised ESR
Rx: NSAIDs
📌 PARA commonly asks:
“”A patient presents with pleuritic chest pain and a low-grade fever 4 weeks after being treated for a STEMI. What is the most likely diagnosis?”
⚠️ Complications
Early: arrhythmias (VT, VF, AF), cardiogenic shock, acute MR (papillary rupture), free wall rupture, pericarditis.
Late: LV aneurysm, heart failure, recurrent MI, Dressler’s syndrome (autoimmune pericarditis weeks later).
🔎 Key PARA Exam Traps
💡 PCI Window: Primary PCI only if it can be delivered within 120 minutes of when fibrinolysis could have been given.
💡 Fibrinolysis Failure: <50% ST-resolution at 60–90 mins → Immediate Rescue PCI.
💡 NSTEMI: Never give fibrinolysis — management is based on the GRACE score.
💡 Biochemical Distinction: UA = normal troponin; NSTEMI = raised troponin.
💡 Oxygen Therapy: Only give O₂ if SpO₂ <94% (<88% in COPD) to avoid coronary vasoconstriction.
💡 Antiplatelet Choice (PCI): Prasugrel first-line unless already on oral anticoagulation → use Clopidogrel.
💡 Age ≥75 Rule: Prasugrel increases bleeding risk — consider Ticagrelor instead.
💡 NSTEMI Timing: GRACE (6-month mortality) >3% → angiography within 72 hours.
💡 Invasive Strategy Trap: Only give Prasugrel in NSTEMI/UA once PCI is intended.
💡 Renal Function: Use Fondaparinux unless Creatinine >265 µmol/L → dose-adjusted UFH.
💡 ACEi Titration: Titrate every 12–24h in hospital; complete within 4–6 weeks post-discharge.
💡 Aldosterone Antagonists: Start 3–14 days post-MI if LVEF ≤40% and symptomatic, after ACEi.
💡 Cardiac Rehab: Assessment within 10 days; programme should start before discharge.
💡 Monitoring Trap: Check U&Es before ACEi/ARB and repeat at 1–2 weeks.
📅 Last updated in line with:
NICE NG185 (2025/26 Consolidated Update): Replacing separate CG167 (STEMI) and NG185 (NSTEMI) targets with a unified ACS “Invasive-First” framework.
ESC ACS Guidelines (2025 Focused Update): Addressing the shift towards P2Y12 inhibitor monotherapy after 1–3 months in high-bleeding-risk patients.
UDMI-5 (2026): The 5th Universal Definition of Myocardial Infarction, emphasizing the Type 1 vs. Type 2 distinction.
PARA/MLA-aligned: Fully reviewed February 2026 for current exam blueprints.
🔒 PASSMAP Assurance: This content is peer-reviewed, NICE-compliant, and optimized for the GMC Medical Licensing Assessment (MLA) and PA National Exam (PARA).
Educational platform. Not medical advice.
