6. Shock & Circulatory Collapse
 Definition
Definition
Shock is a life-threatening state of circulatory failure resulting in inadequate tissue perfusion and cellular hypoxia, leading to end-organ dysfunction and death if untreated.
Shock is classified into four major haemodynamic types:
- Cardiogenic
- Hypovolaemic
- Distributive
- Obstructive
🎯 EXAM ANCHOR – CORE CONCEPT (PARA)
Shock = circulatory failure → inadequate oxygen delivery → organ dysfunction
Hypotension may be absent early
Raised lactate = tissue hypoperfusion
📌 PARA commonly asks:
What defines shock physiologically?
Types of Shock (Classification)
 Mnemonic: “CHOD”
Mnemonic: “CHOD”
Causes (Aetiology)
The causes of shock are best categorized by the haemodynamic mechanism of failure.
1. Cardiogenic (Pump Failure)
Acute Myocardial Infarction: Most common cause (especially anterior MI).
Acute Valvular Dysfunction: e.g., Papillary muscle rupture leading to acute Mitral Regurgitation.
Myocarditis: Viral or inflammatory.
Arrhythmias: Extreme bradycardia (Heart block) or tachycardia (VT/VF).
2. Hypovolaemic (Fluid Loss)
Haemorrhagic: Trauma, Ruptured AAA, Ectopic pregnancy, or massive GI bleed.
Non-haemorrhagic: Severe dehydration, vomiting/diarrhoea, or “Third-spacing” in major burns/pancreatitis.
3. Obstructive (Physical Blockage)
Massive Pulmonary Embolism: Prevents blood reaching the Left Atrium.
Tension Pneumothorax: Mediastinal shift kinks the Great Veins, stopping return to the heart.
Cardiac Tamponade: Fluid in the pericardium prevents the ventricles from filling.
4. Distributive (Vasodilation)
Sepsis: Overwhelming systemic inflammatory response.
Anaphylaxis: IgE-mediated massive histamine release.
Neurogenic: Loss of sympathetic tone following a high Spinal Cord Injury.
 EXAM ANCHOR – CORE CONCEPT (PARA)
EXAM ANCHOR – CORE CONCEPT (PARA)
Type | Primary Problem | Key Examples |
Cardiogenic | Pump failure | MI, severe HF, arrhythmia |
Hypovolaemic | ↓ Preload | Haemorrhage, dehydration |
Distributive | ↓ SVR | Sepsis, anaphylaxis |
Obstructive | Outflow obstruction | PE, tamponade, tension pneumothorax |

Which type of shock is caused by pulmonary embolism?
 Causes (Aetiology)
Causes (Aetiology)
Cardiogenic
-
Acute MI
-
Severe heart failure
-
Malignant arrhythmias
-
Acute valvular failure (e.g. papillary muscle rupture)
Hypovolaemic
-
Haemorrhage (GI bleed, trauma, ruptured AAA)
-
Severe dehydration (vomiting, diarrhoea, burns)
Distributive
-
Sepsis
-
Anaphylaxis
-
Neurogenic shock
Obstructive
-
Pulmonary embolism
-
Cardiac tamponade
-
Tension pneumothorax
Risk Factors
 Mnemonic: “HARD PUMP”
Mnemonic: “HARD PUMP”
-
Haemorrhage / dehydration
-
Acute MI
-
Ruptured aneurysm
-
Drugs (vasodilators, beta-blockers)
-
PE
-
Uncontrolled infection (sepsis)
-
Malignant arrhythmia
-
Pre-existing heart failure
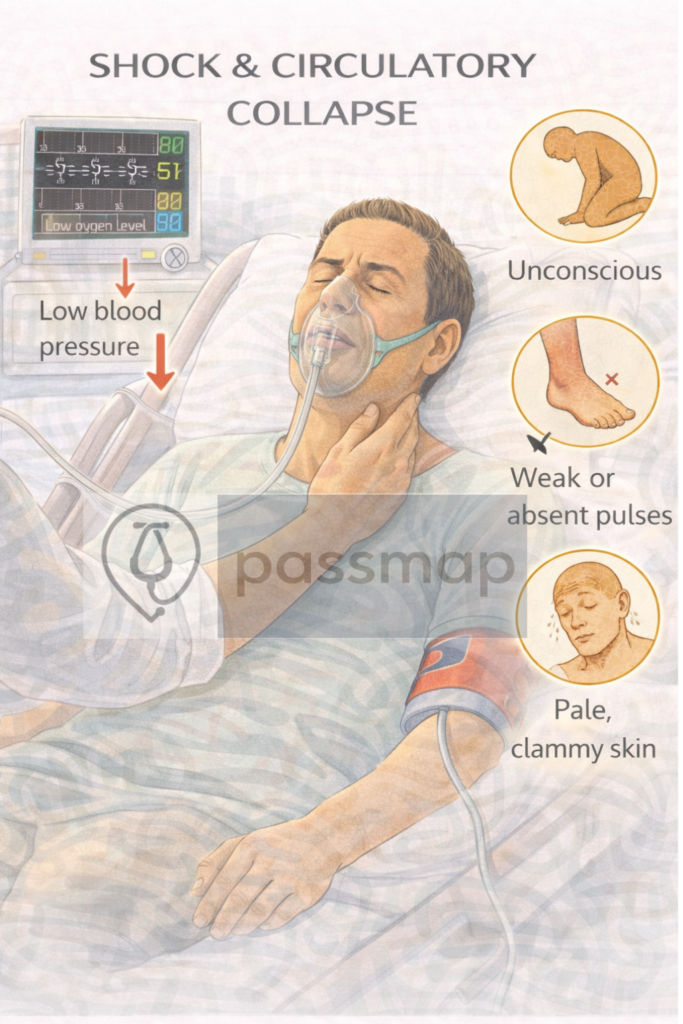
📋 Clinical Features
 Mnemonic: “SHOCKED”
Mnemonic: “SHOCKED”
Systolic BP ↓ or narrow pulse pressure
Hypoxia
Oliguria (<0.5 mL/kg/hr)
Confusion
Kool peripheries (except early septic shock)
Elevated lactate
Diaphoresis / tachycardia
 EXAM ANCHOR – CORE CONCEPT (PARA)
EXAM ANCHOR – CORE CONCEPT (PARA)
- Normal blood pressure does NOT exclude shock
- Early shock = tachycardia + rising lactate
 PARA commonly asks:
PARA commonly asks:
Which laboratory marker indicates tissue hypoperfusion?
 Examination Findings
Examination Findings
-
Tachycardia
-
Hypotension (late sign)
-
Prolonged capillary refill (>2 seconds)
-
Cold clammy skin (except early septic shock)
-
Raised JVP (cardiogenic / obstructive)
-
Reduced urine output
 Investigations
Investigations
First-Line:
|
Investigation |
Purpose |
|---|---|
|
ABG / VBG |
Lactate, metabolic acidosis |
|
Bloods (FBC, U&Es, LFTs, CRP) |
Identify cause |
|
ECG |
MI, arrhythmia |
|
CXR |
PE signs, pulmonary oedema, pneumothorax |
|
Urine output |
Marker of perfusion |
Second-Line
Investigation | When |
|---|---|
Troponin | Suspected cardiogenic shock |
Blood cultures | Suspected septic shock |
CTPA | Suspected PE |
CT Abdomen | Suspected bleeding / ischaemia |
Specialist
Investigation | Use |
|---|---|
Echocardiography | Cardiogenic vs obstructive shock |
CT Mesenteric Angiography | Suspected intestinal ischaemia |
 EXAM ANCHOR – CORE CONCEPT (PARA)
EXAM ANCHOR – CORE CONCEPT (PARA)
- Raised lactate is the most reliable biochemical marker of shock.
 PARA commonly asks:
PARA commonly asks:
Which laboratory marker indicates tissue hypoperfusion?
Management
- Immediate (All Shock)
Mnemonic: “ABCDE + FLUIDS”
- Airway
- Breathing (high-flow oxygen)
- Circulation (2 large-bore IV cannulae)
- Disability (GCS, glucose)
- Exposure
- Fluids (crystalloid bolus unless cardiogenic)
 EXAM ANCHOR – CORE CONCEPT (PARA)
EXAM ANCHOR – CORE CONCEPT (PARA)
Hypovolaemic / septic shock → IV crystalloid
Cardiogenic shock → cautious fluids ± inotropes
 Definitive Treatment (Cause-Specific)
Definitive Treatment (Cause-Specific)
Shock Type | Key Treatment |
|---|---|
Cardiogenic | Treat MI, inotropes, urgent cardiology |
Hypovolaemic | IV fluids ± blood products |
Septic | IV antibiotics within 1 hour |
Anaphylactic | IM adrenaline |
Obstructive | PE thrombolysis, pericardiocentesis |
📌 PARA commonly asks
What is the first-line treatment for septic shock?
 Complications
Complications
-
Acute kidney injury
-
Multi-organ failure
-
ARDS
-
Disseminated intravascular coagulation (DIC)
-
Death
 Red Flags
Red Flags
Lactate ≥2 mmol/L
Persistent hypotension despite fluids
Reduced urine output
Altered mental state
Evidence of end-organ damage
 Differential Diagnoses
Differential Diagnoses
-
Sepsis without shock
-
Acute heart failure
-
Massive PE
-
Severe dehydration
-
Adrenal crisis
Review & Safety Netting
Continuous NEWS2 monitoring
Escalate early to senior / critical care
Reassess response to fluids within 30–60 minutes
 Key PARA Exam Traps
Key PARA Exam Traps
Shock ≠ hypotension
Normal BP does not exclude shock
Lactate rises before BP falls
Cardiogenic shock → fluids can worsen pulmonary oedema
Obstructive shock requires mechanical relief, not fluids alone
 Key PARA Exam Traps
Key PARA Exam Traps






- NICE NG51 – Sepsis recognition, diagnosis and early management
- NICE CG94 – Unstable angina and NSTEMI
- NICE NG158 – Venous thromboembolic diseases
- NICE NG39 – Major trauma
- GMC PARA Curriculum – Cardiovascular emergencies
Last reviewed: February 2026

Educational platform. Not medical advice.
