6. Irritable Bowel Syndrome
 Definition
Definition
IBS (Irritable Bowel Syndrome) is a functional bowel disorder causing recurrent abdominal pain with altered bowel habit.
IBD Subtypes:
- IBS-C constipation-predominant
- IBS-D diarrhoea-predominant /
- IBS-M mixed
- IBS-U unclassified without structural disease.
- Use a positive diagnosis approach (Rome IV criteria)
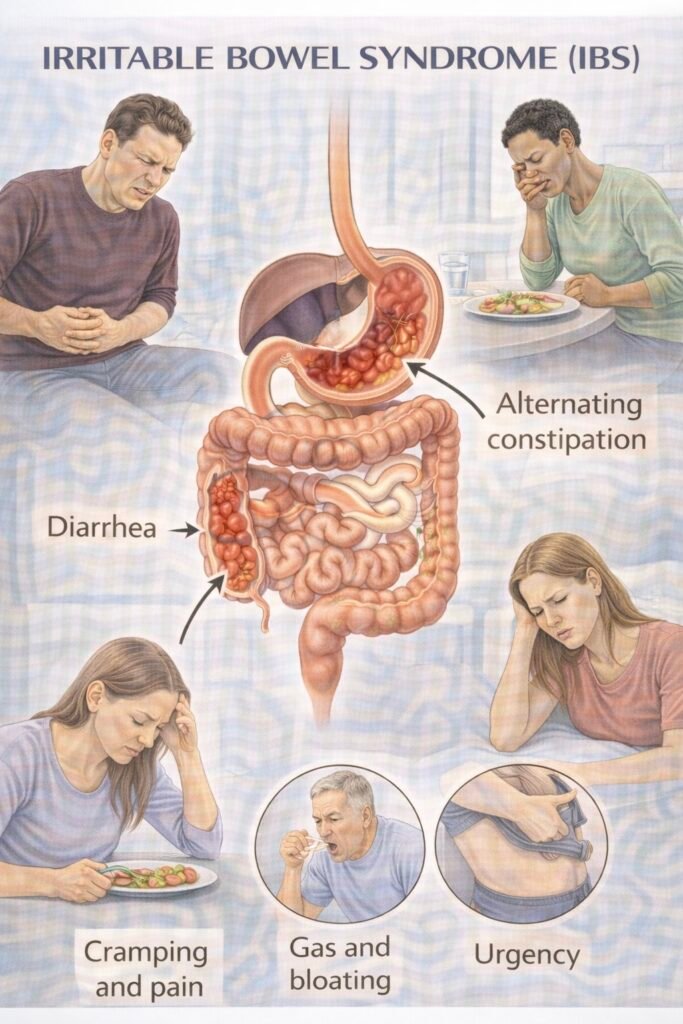
 Clinical features
Clinical features
-
Crampy lower abdominal pain linked to bowel movements
-
Bloating/distension (often post-prandial)
-
Altered habit by subtype:
-
IBS-D: loose stools, urgency, “morning rush”
-
IBS-C: hard stools, straining, incomplete emptying
-
IBS-M: swings hard ↔ loose
-
-
Mucus can occur; nocturnal symptoms uncommon (if waking up from sleep → think organic)
🛡️ Aetiology / Risk Factors
| Domain | Key mechanism | Examples | What you do |
|---|---|---|---|
| Gut–brain axis | Visceral hypersensitivity, altered motility | Stress/anxiety/depression | Education; self-management; low-dose TCA/CBT if persistent pain |
| Post-infectious | After gastroenteritis/antibiotics | “Traveller’s diarrhoea” history | Diet first; loperamide PRN; consider BAD if refractory |
| Dietary triggers | Fermentation/osmotic load → gas/water | High-FODMAPs, caffeine/alcohol/fizzy drinks | Soluble fibre; low-FODMAP (dietitian) if persistent |
| Medicines | Drug-induced C/D | Constipating: opioids, anticholinergics, TCAs, iron, CCBs • Diarrhoea: metformin, Mg | Deprescribe/switch where safe; treat by subtype |
| Hormonal | Cyclical effects | Female, peri-menstrual flares | Symptom diary; optimise around cycle |
| Not IBS (exclude) | Secondary/organic causes | Coeliac, IBD, microscopic colitis, BAD | Follow Investigations + When to Refer |
🧭 When to Refer — Red Flags (and pathways)
| Tier | Key triggers (examples) | Action |
|---|---|---|
| 🚑 Immediate emergency | Obstruction/peritonism • severe dehydration • acute GI bleed | Same-day ED/surgical team |
| ⚡ Urgent suspected cancer – “2WW” | FIT (faecal immunochemical test) ≥10 µg Hb/g OR NG12 (NICE Guideline 12) criteria: e.g., ≥50 with change in bowel habit; IDA (iron-deficiency anaemia); rectal bleeding; palpable mass; ≥40 with weight loss + abdominal pain | CRC (colorectal cancer) 2-week-wait pathway; do not delay if high clinical concern even with a low FIT |
| ⚡ Urgent gastroenterology | Raised faecal calprotectin; nocturnal diarrhoea/weight loss; persistent diarrhoea in older adults; suspected microscopic colitis/BAD; refractory despite ladder | Urgent clinic; targeted tests |
| 📮 Routine | Failure of first/second-line measures; need dietitian-led low-FODMAP or gut-directed CBT | Community/specialist pathways |
DG56 (NICE Diagnostics Guidance 56) explains how to use FIT to guide CRC referral; DG11 covers faecal calprotectin to distinguish IBD vs IBS.
Investigations (to support a positive diagnosis)
| Test | Why / When | How / Notes |
|---|---|---|
| FBC (full blood count) | Screen anaemia/red flags | IDA → consider NG12/2WW pathway rather than IBS |
| CRP / ESR (C-reactive protein / erythrocyte sedimentation rate) | Functional vs inflammatory | Normal supports IBS; raised → IBD/infection |
| Coeliac serology – tTG-IgA + total IgA (tissue transglutaminase IgA) | Exclude coeliac disease | If IgA deficient, use an IgG-based test |
| Faecal calprotectin | Adults with recent-onset lower-GI symptoms when cancer not suspected (IBD vs IBS) | Not needed in classic long-standing IBS without red flags |
| FIT (faecal immunochemical test) | If CRC concern | Refer if FIT ≥10 µg Hb/g; don’t delay if high suspicion |
| TSH (thyroid-stimulating hormone) / serum calcium | If clinically indicated | Not routine for every patient |
| Targeted stool tests | Travel/infectious risk | Use selectively |
Supportive tools: 2-week symptom & stool diary; subtype using the Bristol Stool Form Scale (BSFS):
 BSFS = Bristol Stool Form Scale
BSFS = Bristol Stool Form Scale
Types 1–2 = hard, 3–5 = normal, 6–7 = loose/watery.
 Management — (adults, primary care first)
Management — (adults, primary care first)

Positive diagnosis; explain brain–gut axis. Regular meals; fluids; activity; limit caffeine/alcohol/fizzy drinks; fruit ≤3/day; start 2-week diary.

Soluble fibre (psyllium/ispaghula). Avoid insoluble bran if worse; reduce resistant starch.

-
Pain/bloat: antispasmodic (mebeverine/hyoscine) or peppermint oil.
-
IBS-D: loperamide PRN/titrate.
-
IBS-C: PEG (polyethylene glycol/macrogol); avoid lactulose if bloating.

Low-FODMAP diet (4–6 weeks) with a dietitian, then re-introductions.
Low-dose TCA (e.g., amitriptyline 10 mg nocte; titrate; review at 4–6 weeks). Consider SSRI (selective serotonin reuptake inhibitor) if TCA not tolerated or mood/anxiety dominates.

Linaclotide for refractory IBS-C (specialist-initiated per local pathway).
Gut-directed CBT/psychological therapies.
Assess for BAD, microscopic colitis, or pelvic floor dysfunction if refractory.
🔁 Follow-Up & Monitoring
| Phase | Frequency | Core checks | Escalate if… |
|---|---|---|---|
| Initial/changes | 4–8 weeks | Symptom/stool diary, BSFS type, response & side-effects | No response; red flags emerge |
| Stable | 8–12 weeks | Maintenance plan, flare strategy, lifestyle adherence | Relapse or function declines |
🧠 Memory Boxes
Rome IV “1–3–6”: pain 1 day/week • for 3 months • onset 6 months; +2 (defecation/frequency/form).
Subtype cheat (BSFS): 1–2 hard = C, 6–7 loose = D, >25% both = M, else U.
Diet mantra: Soluble fibre in; insoluble out; low-FODMAP with a dietitian.
Drug picks: Pain → antispasmodic/peppermint, D → loperamide, C → PEG, persistent pain → low-dose TCA.
📅 Last updated
Aligned with NICE CG61 (IBS in adults), DG11 (faecal calprotectin), NG12 (suspected cancer recognition/referral), and DG56 (using FIT for CRC referral).
- PARA-aligned, reviewed February 2026
Educational platform. Not medical advice.
