5. Infection (Bacterial, Viral, Fungal, Tuberculosis)
 Definition
Definition
Respiratory infections involve inflammation of lung tissue due to pathogenic microorganisms, typically categorised as:
Bacterial (e.g. Streptococcus pneumoniae, Haemophilus influenzae)
Viral (e.g. Influenza, RSV, COVID-19)
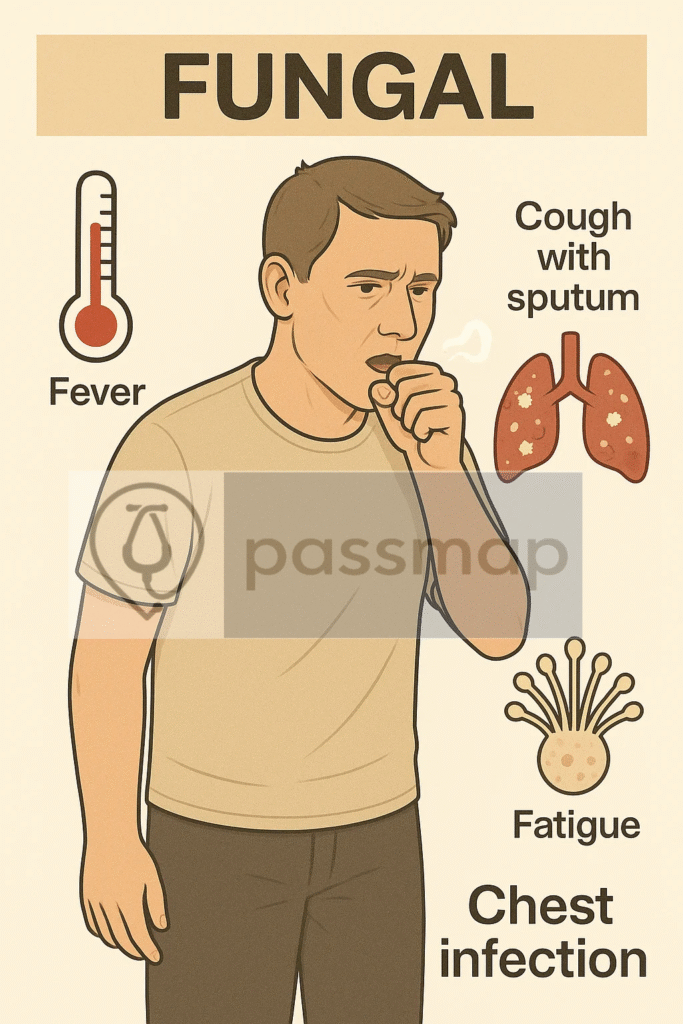
Fungal (e.g. Aspergillus, Pneumocystis jirovecii)
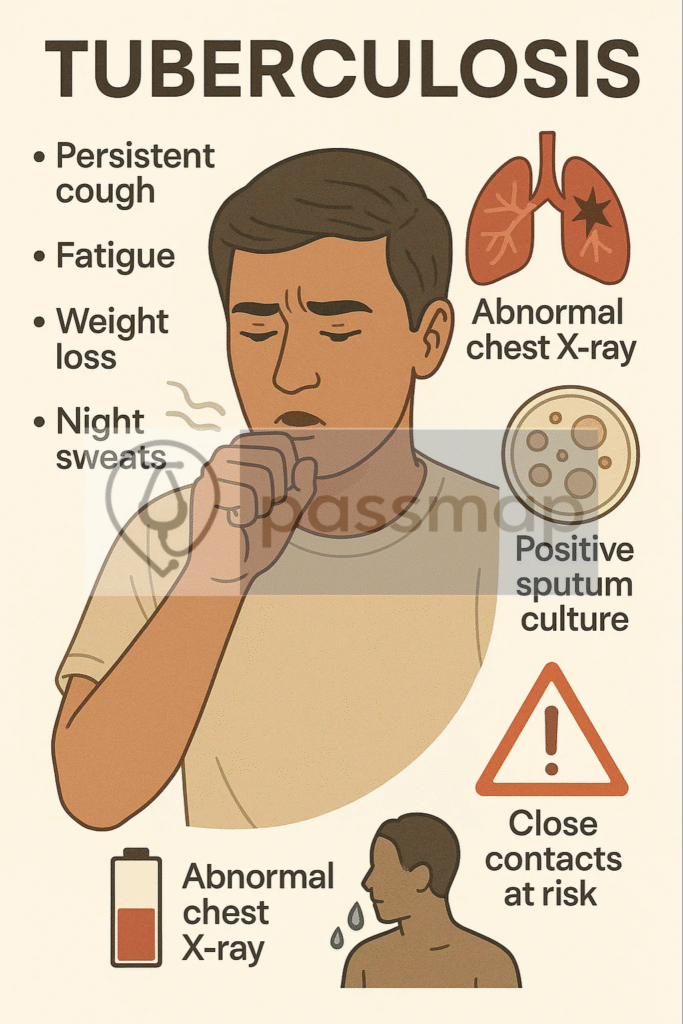
Mycobacterial (Tuberculosis – Mycobacterium tuberculosis)
🎯 EXAM ANCHOR – CORE CONCEPT (PARA)
Respiratory infection = lung inflammation due to pathogenic organisms
Classified as bacterial, viral, fungal, or mycobacterial (TB)
📌 PARA commonly asks:
How are respiratory infections broadly classified?
🛡️Causes (Aetiology)
Mnemonic: “B-FIT”
Bacterial – S. pneumoniae, H. influenzae, Legionella
Fungal – Aspergillosis, Pneumocystis jirovecii
Influenza viruses – Influenza A/B, RSV, COVID-19
Tuberculosis – M. tuberculosis (airborne)
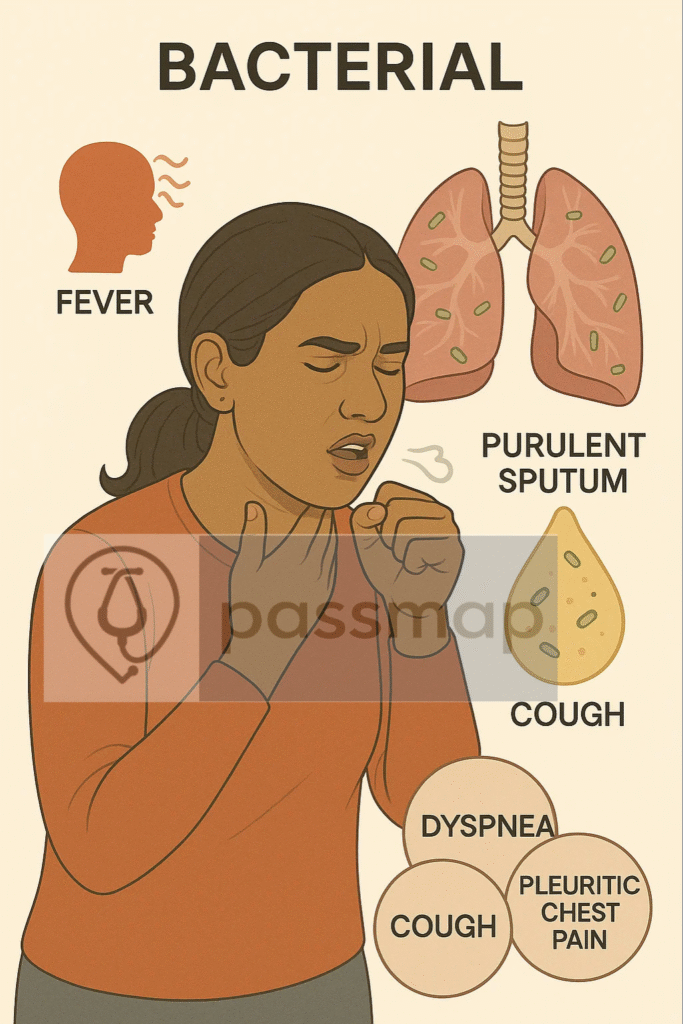
🎯 EXAM ANCHOR – BACTERIAL vs VIRAL (PARA)
Bacterial → acute onset, focal signs, raised CRP/WCC
Viral → diffuse symptoms, bilateral changes, normal/mild WCC rise
📌 PARA commonly asks:
Which features suggest bacterial rather than viral pneumonia?
📋 Risk Factors
🧠 Mnemonic: HOPE SCAR
HIV/immunosuppression
Overcrowding (TB)
Poor vaccination uptake
Elderly
Smoking
Chronic lung disease (e.g. COPD, asthma)
Alcoholism
Recent hospitalisation or travel
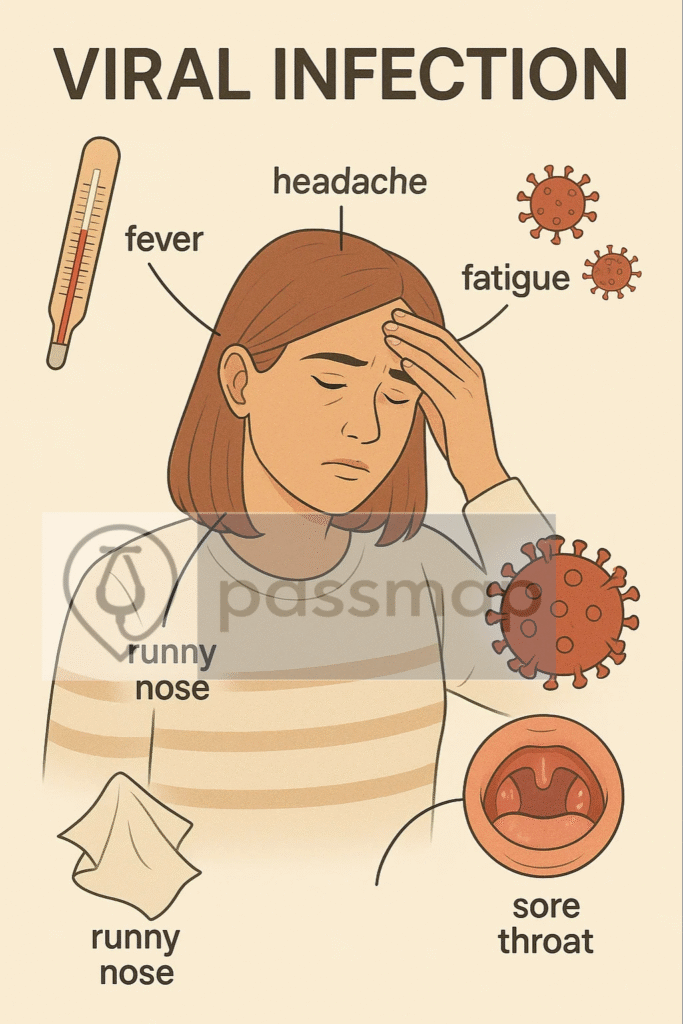
 Clinical Features
Clinical Features

Fever
Exertional dyspnoea
Vomiting/cough +/- sputum
Elevated CRP/WCC
Rales or crepitations on auscultation
Chest pain (pleuritic)
O2 desaturation
Productive cough (± purulent)
Shivering or rigors
 Examination Findings
Examination Findings
-
↓ Chest expansion
-
Dullness to percussion
-
Bronchial breathing or crackles
-
Tracheal deviation (TB cavity/effusion-related)
-
Lymphadenopathy (TB, fungal)
Investigations
| Level | Investigation | When to Use |
|---|---|---|
| 🟢 First-Line | CXR – consolidation, effusion, cavitation | All suspected pneumonia, TB, COVID, fungal infections |
| Bloods – FBC, CRP, U&Es, LFTs | Baseline and inflammatory markers | |
| O2 sats / ABG | Hypoxia, suspected respiratory failure | |
| Sputum culture | Moderate–severe infections or poor response to empiric therapy | |
| PCR (viral swab) | If viral infection suspected (COVID, flu, RSV) | |
| 🟡 Second-Line | Blood cultures | If sepsis suspected or severe pneumonia |
| Procalcitonin | Guide bacterial vs viral aetiology (esp. in hospital) | |
| Tuberculin skin test / IGRA | Suspected TB, especially latent or extrapulmonary | |
| HIV test | All cases of Pneumocystis jirovecii pneumonia or suspected immunosuppression | |
| 🔴 Specialist | HRCT Chest | Suspected fungal lung disease, unresolved pneumonia, cavitary lesions |
| Bronchoscopy + BAL | Immunocompromised, non-resolving pneumonia, suspected TB/fungal disease |
🎯 EXAM ANCHOR – DIAGNOSIS (PARA)
CXR is first-line imaging for suspected pneumonia or TB
Normal CXR does not exclude early TB
📌 PARA commonly asks:
What is the first-line investigation in suspected pneumonia?
🎯 EXAM ANCHOR – MICROBIOLOGY (PARA)
Sputum culture indicated in moderate–severe infection or poor response
Identifies causative organism and resistance
📌 PARA commonly asks:
When should sputum cultures be sent in respiratory infection?
🎯 EXAM ANCHOR – IMMUNOCOMPROMISED HOST (PARA)
- Consider fungal and atypical infections early
- Pneumocystis jirovecii → HIV, raised LDH, hypoxia
📌 PARA commonly asks:
Which infection should be suspected in an immunocompromised patient with hypoxia and diffuse infiltrates?
Severity Assessment (CAP Specific)
📊 CURB-65 Score – NICE NG138 (2023)
| Component | Criteria | Points |
| Confusion | AMT ≤8 | +1 |
| Urea | >7 mmol/L | +1 |
| Respiratory rate | ≥30 breaths/min | +1 |
| Blood pressure | Systolic <90 or Diastolic ≤60 | +1 |
| Age ≥65 | +1 |
Score Interpretation:
0–1: Home treatment
2: Hospital referral
≥3: Urgent hospital + consider ICU
CRB-65 (Primary Care) vs. CURB-65 (Secondary Care)
NICE makes a clear distinction that is frequently tested:
In Primary Care: Use CRB-65 (Urea is unavailable). A score of 1 or more should prompt consideration for hospital referral.
In Secondary Care: Use CURB-65.
Correction: Ensure your summary specifies that Urea is the “hospital-only” component.
Management
🧠 Mnemonic: ABC + PATH
Antibiotics – based on local guidelines & CURB-65
🎯 EXAM ANCHOR – SEVERITY (CAP)
- CURB-65 assesses pneumonia severity
- Guides site-of-care decision
📌 PARA commonly asks:
Which scoring system is used to assess severity in community-acquired pneumonia?
Barrier nursing for TB/COVID
Community vs Hospital admission decision (CURB-65)
Public Health notification (TB, COVID)
Anti-viral/fungal agents if indicated
Treat underlying immunodeficiency
Hydration, oxygen, and supportive care
📝 Example: TB Treatment
6-month RIPE: Rifampicin, Isoniazid, Pyrazinamide, Ethambutol (first 2 months)
Then Rifampicin + Isoniazid (4 months)
- Screening for Latent TB involves IGRA (Interferon-Gamma Release Assay) or Mantoux; Active TB requires Sputum Smears (AFB) and Culture.
TB Medication Side Effects (High-Yield PARA Topic)
PARA almost always asks about their specific toxicities:
Rifampicin: Red/Orange secretions (tears/urine); Cytochrome P450 inducer.
Isoniazid: Peripheral neuropathy (must co-prescribe Vitamin B6/Pyridoxine); Hepatotoxicity.
Pyrazinamide: Hyperuricaemia (can trigger Gout); Hepatotoxicity.
Ethambutol: Optic neuritis (blurred vision/red-green colour blindness). “E for Eye.”
 PARA Decision Matrix: IGRA vs. Mantoux vs. Sputum
PARA Decision Matrix: IGRA vs. Mantoux vs. Sputum
| Test | Best Used For… | PARA Key Fact |
| Mantoux | Initial screening for Latent TB. | Can give false positive if the patient had a BCG vaccine. |
| IGRA | Confirming Latent TB (if Mantoux is positive or if the patient had a BCG). | Highly specific; no false positives from BCG. |
| Sputum Smear/Culture | Diagnosing Active TB. | Requires 3 samples (one early morning). Smear uses Ziehl-Neelsen stain. |
📌 PARA commonly asks:
A patient with suspected TB has had a prior BCG vaccination. Which test is most appropriate to screen for latent infection while minimizing false-positive results?
🎯 EXAM ANCHOR – INFECTION CONTROL (PARA)
TB requires isolation and contact tracing
Infection control decisions are examinable
📌 PARA commonly asks:
Which respiratory infection requires airborne isolation?
 Bacterial & Atypical Pneumonia (The “Host” Clues)
Bacterial & Atypical Pneumonia (The “Host” Clues)
| Organism | PARA Clue (The “Trigger”) | NICE Treatment (UK) |
| S. pneumoniae | Rusty sputum + Lobar consolidation. | Amoxicillin (5 days) |
| L. pneumophila | Hyponatraemia + Travel + Deranged LFTs. | Clarithromycin |
| M. pneumoniae | Young + Erythema Multiforme (Target rash). | Clarithromycin |
| S. aureus | Worsening immediately after Flu recovery. | Flucloxacillin |
| Klebsiella | Alcoholic + “Red currant jelly” sputum. | Cefotaxime |
| HAP (>48h) | Hospitalized patient + new fever/cough. | Tazocin |
🤧 Viral & Fungal (The “Host” Clues)
| Infection | PARA Clue (The “Trigger”) | NICE / UK Management |
| PCP | HIV + Desaturation on exertion + ↑LDH. | Co-trimoxazole |
| Aspergillus | Immunosuppressed + Haemoptysis + Cavity. | Voriconazole |
| Influenza | Abrupt onset, myalgia, headache. | Supportive (± Oseltamivir) |
🏔️ Tuberculosis (The “Safety” Clues)
| Drug | PARA Toxicity (The “Fail” Point) | Mandatory Intervention |
| Rifampicin | Orange urine/tears (P450 Inducer). | Warn patient. |
| Isoniazid | Peripheral neuropathy. | Give Vitamin B6. |
| Pyrazinamide | Gout (Hyperuricaemia). | Monitor Uric Acid. |
| Ethambutol | Optic Neuritis (Red-green color loss). | Baseline Visual Acuity. |
Red Flags
Rapid deterioration
Sepsis/shock
Haemoptysis or cavitation
Multi-lobar involvement
Unresponsive to antibiotics after 48–72h
⚠️ Complications
Lung abscess
Empyema
Sepsis / ARDS
Cavitation (TB)
Bronchiectasis (post-infective)
Differential Diagnoses
PE
Lung cancer
Heart failure
Pneumothorax
Autoimmune ILD
✅ Review & Safety Netting
Always assess for deterioration: NEWS2
Escalate if CURB-65 ≥2 (hospital referral)
Contact tracing for TB
🔎 Key PARA Exam Traps
💡 Bacterial pneumonia → acute onset, fever, focal chest signs, raised CRP/WCC
💡 Viral pneumonia → diffuse symptoms, bilateral infiltrates, normal or mildly raised WCC
💡 CRP is non-specific → indicates inflammation, not organism
💡 Sputum cultures should be sent before antibiotics in severe
💡 Vitamin B6 (Pyridoxine) is given with Isoniazid to prevent peripheral neuropathy.” or recurrent infection
💡 Failure to respond to antibiotics → think resistant organism, wrong diagnosis, or complication
💡 Immunocompromised patients → consider atypical and fungal infections early
💡 Fungal infection (e.g. Aspergillus) → haemoptysis, cavitation, immunosuppression history
💡 TB presents insidiously → weight loss, night sweats, haemoptysis, upper-lobe disease
💡 Normal CXR does not exclude early TB
💡 Always assess infection control risk (TB isolation is an exam favourite)

-
NICE NG138 – Community-acquired pneumonia in adults
-
NICE NG33 – Tuberculosis
-
NICE NG186 – COVID-19 rapid guideline
-
NICE NG164 – Fungal infections: risk prediction and management in critically ill
Published: March 2020 • Last updated: May 2023
Last reviewed: February 2026
Educational platform. Not medical advice.
