5. Constipation
📄 Definition
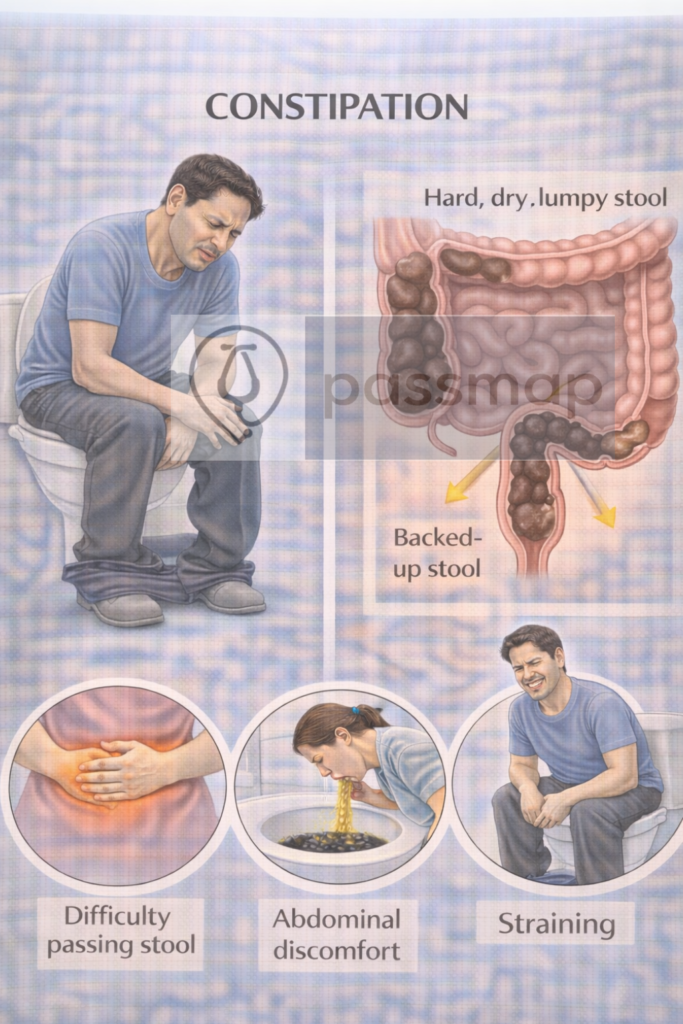
Infrequent and/or difficult stool passage (often <3/week, straining, hard stools), with or without abdominal discomfort. Distinguish primary/functional (slow transit, pelvic floor dyssynergia) from secondary (medications, endocrine/metabolic, neurological).
🛡️ Aetiology / Risk Factors (adult focus)
Meds: opioids, anticholinergics, TCAs, iron, CCBs
Medical: hypothyroidism, hypercalcaemia, diabetes, Parkinson’s, MS
Lifestyle: low fibre/fluids, immobility; pregnancy & older age
Children: withholding, painful fissure history, toilet training issues (see paeds ladder).
🤒 Clinical Features
Hard stools, straining, incomplete emptying, bloating
Alarm features → see 🚩 Red Flags below
Bristol Stool Chart helps standardise stool form (Types 1–7; 3–4 ideal).
🚩 Red Flags (assess first)
Acute obstruction: severe colicky pain, vomiting, distension, absolute constipation
Suspected colorectal cancer: change in bowel habit, rectal bleeding, IDA, abdominal/rectal mass, weight loss → use FIT to guide referral (≥ 10 µg Hb/g).
🔬 Investigations (targeted)
Usually clinical; medication review essential
If indicated: FBC, TFTs, calcium, glucose; FIT per NG12/DG56; DRE (not in suspected abuse/YP without indication).
 Management — Adults
Management — Adults










🧭 When to Refer — Table
| Tier | Key triggers (examples) | Action |
|---|---|---|
| 🚑 Immediate emergency | Suspected obstruction/peritonism; haemodynamic instability; severe rectal pain with fever (abscess) | Same-day ED/surgical review |
| ⚡ 2WW suspected cancer (NG12/DG56) | FIT ≥10 µg Hb/g or age-specific NG12 criteria (e.g., ≥50 with unexplained rectal bleeding; ≥60 with change in bowel habit or IDA; ≥40 with unexplained weight loss + abdominal pain) | 2-week-wait CRC pathway; do not delay if strong concern despite low/absent FIT |
| ⚡ Urgent gastro/colorectal | Persistent impaction not responding; recurrent obstructive symptoms; refractory constipation; suspected pelvic floor dyssynergia | Urgent clinic + targeted tests |
| 📮 Routine | Ongoing symptoms despite stepwise therapy; need biofeedback/dietetic optimisation | Community gastro/physio/dietitian pathway |
 Memory Boxes
Memory Boxes
“POO FIT” (foundations): Position (knees up) • Optimise Output (fibre/fluids) • FIT if cancer features.
“PEG → +Stim → PRU” (ladder): PEG first • add Stimulant • consider PRU calopride if refractory.
Bristol quick recall: 1–2 = hard/slow, 3–4 = ideal, 5–7 = loose/fast.
OIC: “PAMORA if laxatives fail” (naloxegol, naldemedine)
🔁 Follow-Up & Monitoring (Primary Care)
| Phase | Frequency | Core monitoring | Escalate if… |
|---|---|---|---|
| Titration | 2–4 weeks | Symptom diary, Bristol type, laxative dose, side-effects | No response, pain/distension, red flags |
| Stable | 6–12 weeks | Bowel habit, fibre/fluid, meds review | Relapse or dependence on rescue stimulant |
| Weaning | After 2–4 wks of comfortable, regular stools | Gradually reduce laxatives | Recurrence of hard stools/straining |
📅 Last updated in line with
NICE CG99 (Constipation in children and young people) — current online guideline.
NICE CKS – Constipation (Adults) — current topic overview/management.
NICE NG12 (Suspected cancer: recognition and referral) & DG56 (FIT to guide referral) — CRC pathways/FIT ≥10 µg Hb/g.
NICE TA211 (Prucalopride), TA345 (Naloxegol), TA651 (Naldemedine).
- PARA-aligned, reviewed February 2026
PASSMAP ensures all content is NICE-aligned and reviewed for PARA success.
Educational platform. Not medical advice.
