3. Eating Disorders
 Definition
Definition
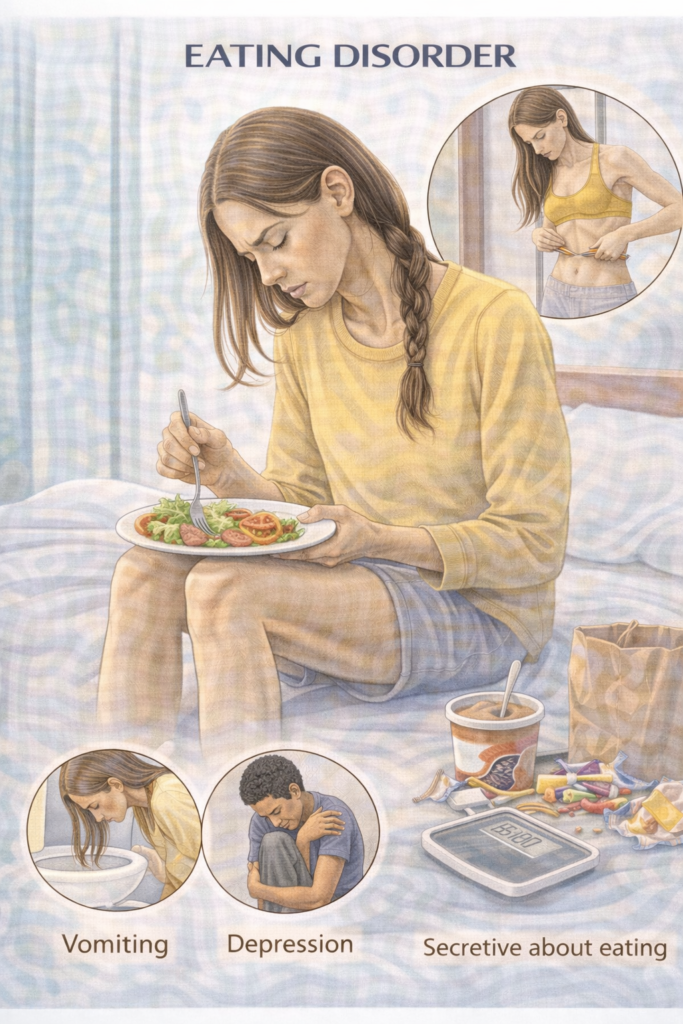
Mental health conditions characterised by abnormal eating behaviours, distorted body image, and often harmful effects on physical health, nutritional status, and psychosocial function.
📂Main Types
Anorexia Nervosa (AN)
Bulimia Nervosa (BN)
Binge Eating Disorder (BED)
Avoidant/Restrictive Food Intake Disorder (ARFID)
Other Specified Feeding or Eating Disorders (OSFED)
📊Epidemiology
Peak onset: adolescence/young adulthood
Female:male ratio ~10:1 (AN & BN)
Increasing prevalence in males and mid-life adults
High psychiatric comorbidity (depression, anxiety, OCD)
🛡️Aetiology / Risk Factors
BIO-PSYCHO-SOCIAL mnemonic
Biological: genetic predisposition, neurochemical (serotonin/dopamine)
Illness history: early GI disorders, Type 1 diabetes (insulin misuse risk)
Obesity history (risk for BED & BN)
Psychological: perfectionism, low self-esteem, body dissatisfaction
Social: bullying, media pressure, cultural ideals
Youth stress: school/relationship stressors
Childhood trauma: abuse, neglect
Home/family dynamics: controlling or critical parenting
Occupational pressures: sports, dance, modelling
Life transitions: puberty, moving away from home
 Clinical Features
Clinical Features
1. Anorexia Nervosa
Restriction of energy intake → significantly low body weight
Intense fear of gaining weight
Distorted body image
Physical signs: amenorrhoea, lanugo hair, bradycardia, hypotension, hypothermia
2. Bulimia Nervosa
Recurrent binge eating + compensatory behaviours (vomiting, laxatives, excessive exercise)
Self-evaluation unduly influenced by body shape/weight
Often normal weight or overweight
Physical signs: dental erosion, parotid swelling, Russell’s sign (knuckle scars)
3. Binge Eating Disorder
Recurrent binge episodes without compensatory behaviours
Marked distress, rapid eating, eating when not hungry
4. ARFID
Avoidance/restriction of food intake not due to body image concerns
Leads to nutritional deficiency, weight loss, dependency on supplements
⚠️Complications
HEART mnemonic (high-yield for exams)
Hypokalaemia (BN → arrhythmia risk)
Endocrine: amenorrhoea, osteoporosis
Arrhythmias, prolonged QT
Reproductive issues: infertility
Total body protein loss → muscle wasting
🧪Investigations
(Assess medical stability & exclude organic causes)
Bloods: FBC, U&E (K+, Na+, phosphate), LFTs, TFTs, glucose, magnesium, vitamin B12, folate
ECG: bradycardia, QT prolongation
Bone density scan (DEXA): osteoporosis risk (AN)
Screen for comorbidities: depression, anxiety, substance misuse
 Malnutrition & Nutritional Risk (Adults & YP)
Malnutrition & Nutritional Risk (Adults & YP)
Screen & grade risk early (same day):
Adults: use MUST (BMI, % weight loss, acute disease effect). Score 0 = low, 1 = medium, ≥2 = high → act accordingly. Dietitian referral if ≥1 or any clinical concern. BAPEN
Children/Young people: plot weight/height/BMI centiles, look for centile crossing / growth faltering and clinical red flags (bradycardia, hypotension, electrolyte disturbance). NICE
High-risk features (trigger MDT & urgent plan):
Very low BMI/centile, rapid recent loss, negligible intake >5 days, or purging with abnormal labs.
Management – NICE NG69 (2024)
General Principles
-
Early intervention
-
Patient-centred, non-judgemental approach
-
Avoid focusing solely on weight/BMI
-
Involve family if appropriate (especially under 18s)
1. Psychological Treatment
-
Anorexia Nervosa (Adults): Individual eating disorder-focused CBT (CBT-ED) or Maudsley Anorexia Nervosa Treatment for Adults (MANTRA)
-
Bulimia Nervosa / BED: CBT-ED first-line
-
Children/Young people: Family-based therapy (FBT)
2. Medical Monitoring
-
Weekly monitoring if medically unstable
-
Check weight, vitals, and electrolytes
-
Consider admission if high medical risk (see MARSIPAN criteria: e.g. BMI < 13 in adults, severe electrolyte disturbance, arrhythmia)
3. Dietetic Support
-
Structured meal plans
-
Gradual refeeding (risk of refeeding syndrome – monitor phosphate, magnesium, potassium)
Start low, go slow; replace K⁺/Mg²⁺/PO₄³⁻ alongside feeding; check labs daily initially; ECG if QT/electrolyte issues.
4. Pharmacological
-
No medication as sole treatment
-
BN/BED: fluoxetine may help reduce binge/purge frequency
-
Manage comorbid depression/anxiety
🚩MARSIPAN – Management of Really Sick Patients with Anorexia Nervosa
(Royal College of Psychiatrists & NICE NG69, updated 2024)
Mnemonic: “BRAVE LOSS”
B – Bradycardia (<40 bpm)
R – Rapid weight loss (>1 kg/week)
A – Arrhythmia or prolonged QT on ECG
V – Very low BMI (<13) or <0.4th centile (children)
E – Electrolyte disturbance (K+, phosphate, magnesium)
L – Low blood pressure (<90 systolic) / postural drop >20 mmHg
O – Organ failure signs (liver, renal, cardiac)
S – Suicidal intent or severe psychiatric risk
S – Severe hypothermia (<35°C)
 Table – MARSIPAN High-Risk Indicators (Adults)
Table – MARSIPAN High-Risk Indicators (Adults)
| Category | Indicator | Threshold |
|---|---|---|
| Anthropometric | BMI | <13 |
| Weight change | Rapid weight loss | >1 kg/week |
| Cardiovascular | Bradycardia | <40 bpm |
| Systolic BP | <90 mmHg or >20 mmHg postural drop | |
| Arrhythmia | Any clinically significant arrhythmia or prolonged QT | |
| Metabolic | Electrolytes | K+, phosphate, magnesium low |
| Temperature | Hypothermia | <35°C |
| Organ function | Failure | Liver, renal, cardiac compromise |
| Mental health | Suicide risk | Active suicidal intent / severe psychiatric instability |
| Growth (children) | BMI centile | <0.4th centile |
 Electrolyte reference ranges (adults)
Electrolyte reference ranges (adults)
| Analyte | Reference range | Low | Severely low | Notes for PARA |
|---|---|---|---|---|
| Potassium (K⁺) | 3.5–5.3 mmol/L | <3.5 | Treat causes; ECG monitor if <3.0 or symptomatic. | |
| Phosphate (PO₄³⁻) | 0.80–1.50 mmol/L | <0.80 | In refeeding, replace early and monitor daily initially. | |
| Magnesium (Mg²⁺) | 0.70–1.00 mmol/L | <0.70 | HypoMg makes K⁺ repletion harder—replace Mg²⁺ too. |
🧭 When to Refer (Adults & Young People)
| Tier | Key triggers (examples) | Action / destination |
|---|---|---|
| 🚑 Immediate emergency admission (medical) | Any BRAVE LOSS criterion; K⁺ <3.0, PO₄³⁻ <0.3, Mg²⁺ <0.5; QT/arrhythmia; syncope/dehydration; pregnancy with instability; YP with shock, growth faltering, or unsafe at home | Same-day admission via ED/acute med/paediatrics; continuous monitoring; urgent electrolyte replacement; senior review; follow MEED/MARSIPAN pathways |
| ⚡ Urgent specialist (same/next working day) | Marked malnutrition; daily purging + abnormal labs; T1DM with suspected insulin restriction; persistent ECG/lab abnormalities despite initial correction; pregnancy but currently stable; YP with concerning vitals/trajectory | Rapid referral to specialist ED service / CAMHS / paediatrics; repeat labs 24–48 h; safety-net plan |
| 📮 Routine community ED service | Suspected AN/BN/BED/ARFID without red flags; BN/BED not improving after 4–6 weeks guided self-help/CBT-ED; ARFID with nutritional impact (dietitian/SLT/psych) | Refer to community ED team; start/continue CBT-ED principles; involve dietitian/SLT; review in 2–4 weeks |
| 👶 YP/CAMHS note | CAMHS = specialist child/YP MH service; GP usually refers; use local MEED colour pathway; centiles guide monitoring and care setting | Follow local CAMHS/MEED pathway; set review frequency and site (community vs paeds/inpatient) by risk colour |
Safeguarding: Consider at every contact (covert vomiting, laxatives/diuretics, family/carer dynamics, capacity/consent).
🔁 Follow-Up & Monitoring (Outpatients)
| Phase | Frequency | Core monitoring | Extras / when indicated |
|---|---|---|---|
| Early / Unstable | Weekly (or more often) | Vitals: lying/standing BP/HR, temp • Weight/BMI (or centiles in YP) • U&E, Mg²⁺, PO₄³⁻ | ECG if brady/QT/electrolyte issues or QT-affecting meds • Review nutrition plan and adherence |
| Active Treatment | Every 2–4 weeks | Vitals • Weight/BMI/centiles • U&E, Mg²⁺, PO₄³⁻ (spacing out if stable) | Check purging behaviours, laxatives/diuretics • Psych risk & crisis plan • Medication efficacy/tolerability |
| Consolidation | Monthly × 3–6 | Vitals • Weight/BMI/centiles • Labs if clinically indicated | DEXA if prolonged low weight • Dental review (BN) • Return-to-activity/PE advice |
| Maintenance / Relapse Prevention | Every 3 months (individualise) | Weight trend • Functioning • Brief risk screen | Relapse plan refresh • Dietetic top-ups PRN |
| ➡️ Step-up triggers (escalate per 🧭 When to Refer) | — | Weight falling, vitals/labs worsening, persistent purging, therapy non-engagement, syncope, arrhythmia/QT, pregnancy concerns | Move to ⚡ urgent or 🚑 emergency pathway as appropriate |
 Memory Box — Electrolytes (Key Performance Measures)
Memory Box — Electrolytes (Key Performance Measures)
Key:
K⁺ — “Banana 3–5 rule” → 3.5–5.3 mmol/L (Flip trick: the decimals .5 ↔ .3 (3.5 to 5.3)
Performance:
PO₄³⁻ — “phos-ATE to one-five” → 0.8–1.5 mmol/L
Measures:
Mg²⁺ — “MAG-7 to ONE” → 0.70–1.00 mmol/L

K⁺ <2.5 • PO₄³⁻ <0.3 • Mg²⁺ <0.5 → urgent replacement + ECG monitoring
PARA one-liner:
“K three-to-five; Phos point-eight to one-five; Mag point-seven to one; severe lows 25–03–05.”
 Exam tip:
Exam tip:
PARA likes “red flag” escalation criteria – know both numeric thresholds and the principle (any physiological instability = urgent hospital admission).
In clinical stations, mention MARSIPAN explicitly when discussing high-risk AN management – it shows guideline-based thinking.
Last updated in line with NICE NG69 (Eating disorders: recognition and treatment)
Published: May 2017 • Last updated: May 2024
- PARA-aligned, reviewed February 2026
PASSMAP ensures all content is NICE-aligned and reviewed for Physician Associate Registration Assessment (PARA) success.
Educational platform. Not medical advice.
