3.3. Lymphatic Disorders
📄 Definition
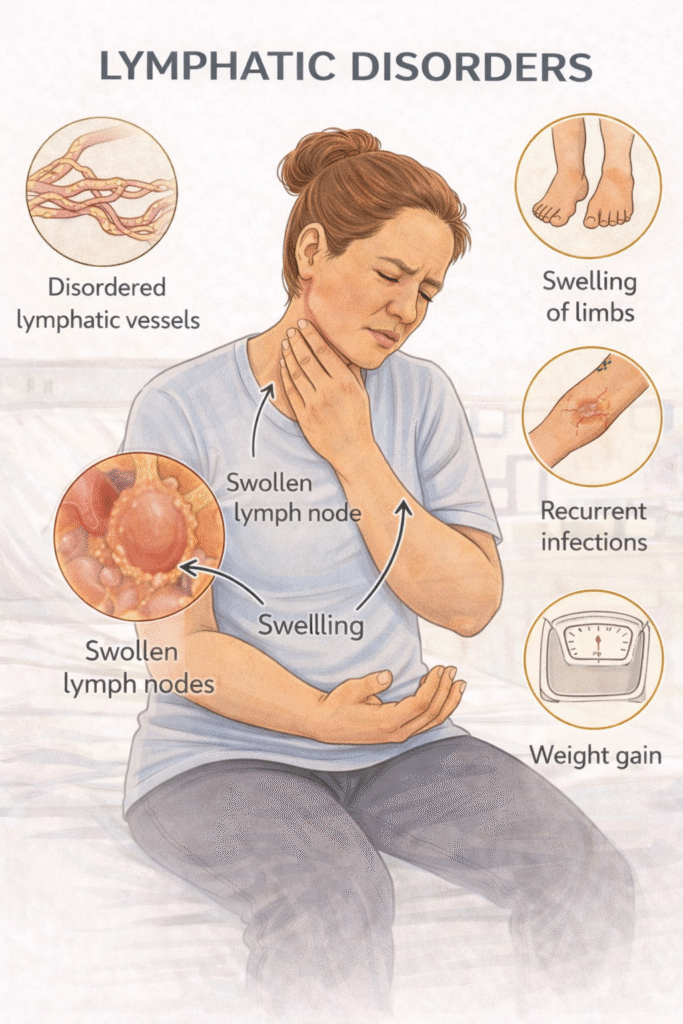
Lymphatic disorders refer to impaired lymphatic drainage, leading to lymphoedema—a chronic, progressive swelling due to the accumulation of lymph fluid in the interstitial space.
It may be primary (congenital or idiopathic) or secondary (damage to lymphatic vessels from surgery, radiotherapy, infection, malignancy).
🧬 Classification
Primary Lymphoedema
Congenital (Milroy disease – presents at birth)
Praecox (Meige disease – adolescence onset)
Tarda (onset >35 years)
Secondary Lymphoedema
Cancer treatment – surgery or radiotherapy
Infection – filariasis (common in tropical regions)
Obesity – mechanical compression
Chronic venous insufficiency – venous overload impairs lymphatics
Trauma or recurrent cellulitis
Risk Factors – Mnemonic: SLOW FLUID
Surgery (lymph node dissection)
Lymphatic malformation (primary)
Obesity
Wounds or trauma
Filariasis (tropical parasitic infection)
Late-stage cancer
Ulceration or infection
Immobility
Deep vein thrombosis history
📋 Clinical Features – Mnemonic: LEGS SWELL
Localised swelling – usually in one or both lower limbs
Early pitting, becomes non-pitting over time
Gradual onset
Skin thickening – “peau d’orange” appearance
Stammering folds or squaring of toes (positive Stemmer’s sign)
Weeping (lymphorrhoea) in severe cases
Eczema – dry, flaky skin prone to infection
Lymphangitis or cellulitis risk
Limb heaviness or aching
Investigations
🥇 First-Line
Clinical examination – look for signs and distribution
ABPI – before applying compression therapy
History – rule out malignancy, DVT, or prior interventions
🥈 Second-Line (if diagnostic uncertainty)
Lymphoscintigraphy – maps lymphatic flow
MRI/CT – if malignancy or obstruction suspected
Ultrasound – assess soft tissue or exclude DVT
Management – Mnemonic: LEMON
Lifestyle – elevate limbs, moisturise, prevent trauma
Exercise – promotes lymphatic flow
Manual lymphatic drainage – by trained specialist
Ongoing compression therapy – multilayer bandaging or stockings (class II–III)
Note infections – early antibiotics for cellulitis
✅ Specialist referral if:
Diagnostic uncertainty
Sudden deterioration
Suspected malignancy
Severe disfigurement
⚠️ Complications
Recurrent cellulitis or lymphangitis
Ulceration
Psychosocial distress
Lymphangiosarcoma (rare but serious)
🔺 Last updated in line with NICE CKS – Lymphoedema
Published: January 2018 • Last updated: August 2023
- PARA-aligned, reviewed February 2026
✅ PASSMAP ensures all content is NICE-aligned and reviewed for Physician Associate Registration Assessment (PARA) success.
Educational platform. Not medical advice.
