2. Empyema
📄 Definition
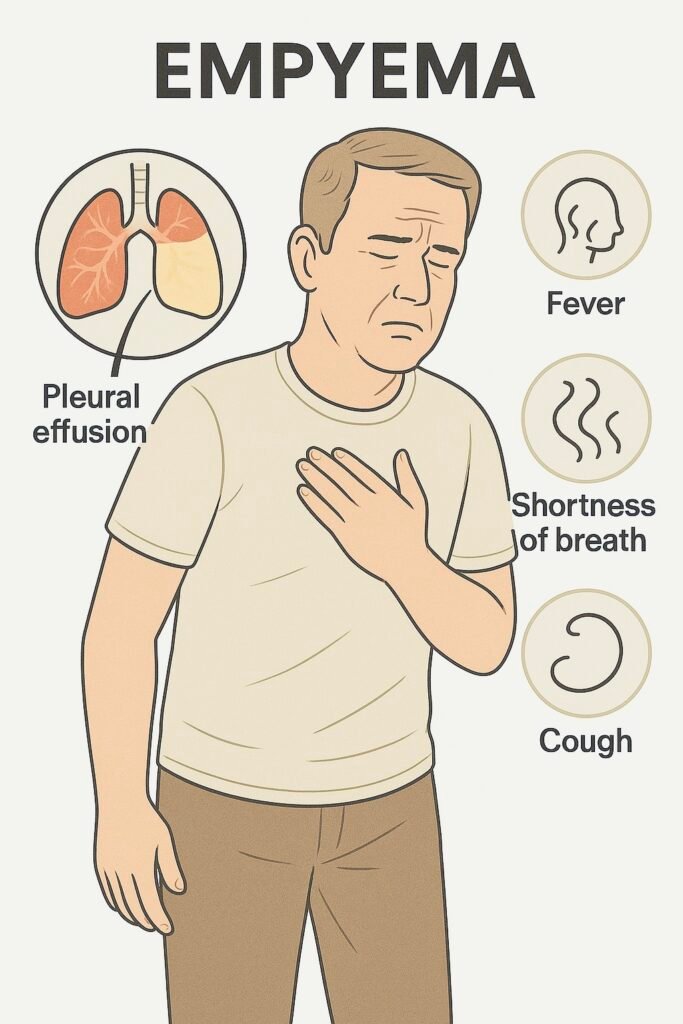
Empyema = pus in the pleural space,
Almost always secondary to complicated pneumonia, chest surgery, trauma, or oesophageal rupture.
🛡️ Causes
🧠 Mnemonic: PECS
-
Pneumonia (bacterial – most common: Strep pneumoniae, Staph aureus, anaerobes)
-
Esophageal rupture (Boerhaave’s, iatrogenic)
-
Chest surgery / trauma
-
Seeding from bloodstream (sepsis, TB)
🔬 Pathophysiology
-
Parapneumonic effusion → infection → neutrophils + bacteria accumulate
-
Fibrin deposition → loculations
-
Formation of thick pus → restricts lung expansion
-
Can → sepsis, respiratory failure, chronic fibrothorax
🔍 Clinical Features
🧠 Mnemonic: PUS FLUID
-
Persistent fever despite antibiotics
-
Unilateral pleuritic chest pain
-
Shortness of breath
-
Foul-smelling sputum / purulent pleural fluid
-
Leukocytosis (↑WCC, ↑CRP)
-
Usually secondary to pneumonia
-
Irritability (esp. in children)
-
Dullness to percussion + ↓ breath sounds
🔬 Investigations
| Step | Investigation | Key Findings / Exam Notes |
|---|---|---|
| 1️⃣ First-line | CXR | Blunted costophrenic angle, meniscus sign |
| Bloods | FBC ↑WCC, CRP ↑, blood cultures | |
| 2️⃣ Confirmatory | Ultrasound chest (US) | Detects loculations, guides aspiration |
| Diagnostic aspiration | Send pleural fluid for pH, glucose, LDH, protein, Gram stain, culture | |
| 3️⃣ Advanced / problem-solving | CT chest | Defines extent, identifies bronchopleural fistula, guides surgery |
📊 Light’s Criteria – Exudate vs Transudate
🧠 Mnemonic: “Protein & LDH Light it up”
| Criterion | Empyema Characteristic |
|---|---|
| Pleural:serum protein >0.5 | Yes → exudate |
| Pleural:serum LDH >0.6 | Yes → exudate |
| Pleural LDH >⅔ ULN | Yes → exudate |
Pleural pH <7.2 strongly suggests empyema → needs drainage.
⚖️ Parapneumonic Effusion vs Empyema
| Feature | Simple Parapneumonic Effusion | Empyema |
|---|---|---|
| Fluid | Sterile, clear | Frank pus / turbid |
| pH | >7.3 | <7.2 |
| Glucose | Normal | <3.3 mmol/L |
| LDH | Mildly ↑ | Very high |
| Management | May resolve with abx | Requires drainage + abx |
💊 Management (Stepwise: BTS/NICE)
| Step | Treatment | Notes |
|---|---|---|
| 1️⃣ First-line | IV antibiotics | Co-amoxiclav, or ceftriaxone + metronidazole. Tailor to culture. |
| 2️⃣ Definitive | Chest tube drainage (US/CT-guided) | Required in almost all empyemas |
| 3️⃣ If loculated / poor drainage | Intrapleural fibrinolytics (tPA + DNase) | Breaks down fibrin septations |
| 4️⃣ Refractory / severe | VATS or thoracotomy + decortication | Indicated if persistent sepsis, trapped lung |
| 5️⃣ Support | Nutrition, fluids, oxygen, analgesia | Especially in children & frail adults |
🧠 Mnemonic: PUS OUT
Pleural drainage (chest tube = definitive)
Ultrasound guidance (confirm & guide insertion)
Systemic antibiotics (start immediately, IV broad → culture-guided)
Optimise nutrition & supportive care
Use fibrinolytics (tPA/DNase if loculated)
Thoracics referral (VATS/decortication if refractory)
⚠️ Complications
Bronchopleural fistula
Fibrothorax (restrictive lung disease)
Sepsis / shock
Respiratory failure
Recurrent empyema
📅 Follow-up
Repeat imaging to confirm resolution
Continue antibiotics 2–6 weeks depending on response
Consider TB testing if high risk
Respiratory review ± surgical follow-up
🔎 Key PARA Exam Traps
💡 pH <7.2 = drain → don’t just “give antibiotics”
💡Ultrasound = first choice to confirm & guide aspiration (not CT)
💡 Light’s criteria = exudate but pH is most specific for empyema
💡 IV antibiotics + chest tube are both required → abx alone never enough
💡 tPA/DNase = exam favourite for multiloculated cases
Last updated in line with BTS Pleural Disease Guidelines & NICE Pneumonia NG138
Published: December 2018 • Last updated: August 2022
- PARA-aligned, reviewed February 2026
PASSMAP ensures all content is NICE-aligned and reviewed for Physician Associate Registration Assessment (PARA) success.
