15. Alcoholism
 Definition
Definition
Chronic, harmful use of alcohol leading to physical, psychological, and social impairment. Strong association with liver disease, GI disorders, mental health conditions, and increased mortality.
 Risk Factors
Risk Factors
Family history (genetic predisposition).
Mental health: depression, anxiety, trauma, social isolation.
Social: unemployment, deprivation, peer culture.
Biological: male sex, early onset drinking.
 Epidemiology (UK)
Epidemiology (UK)
~25% of adults drink above recommended limits (ONS, 2023).
Higher prevalence in men (2× risk).
↑ Burden in Scotland & Northern England.
Ethnicity: ↑ risk in White British; lower in South Asian Muslim populations (religious abstinence).
Alcohol-related hospital admissions: >980,000/year in England.
🔬 Pathophysiology (simplified)
Ethanol → metabolised in liver (alcohol dehydrogenase → acetaldehyde → acetate).
Excess acetaldehyde → toxic to hepatocytes → oxidative stress, inflammation.
Steatosis → steatohepatitis → fibrosis → cirrhosis → HCC.
CNS effects: GABA agonism (sedation) + NMDA antagonism (withdrawal hyperexcitability).
Dependence: altered reward pathways (dopamine, glutamate).
🔍 Clinical Features
🧠 Mnemonic: CAGE
Cut down (felt need to).
Annoyed by criticism.
Guilty about drinking.
Eye-opener drink in morning.
Other:
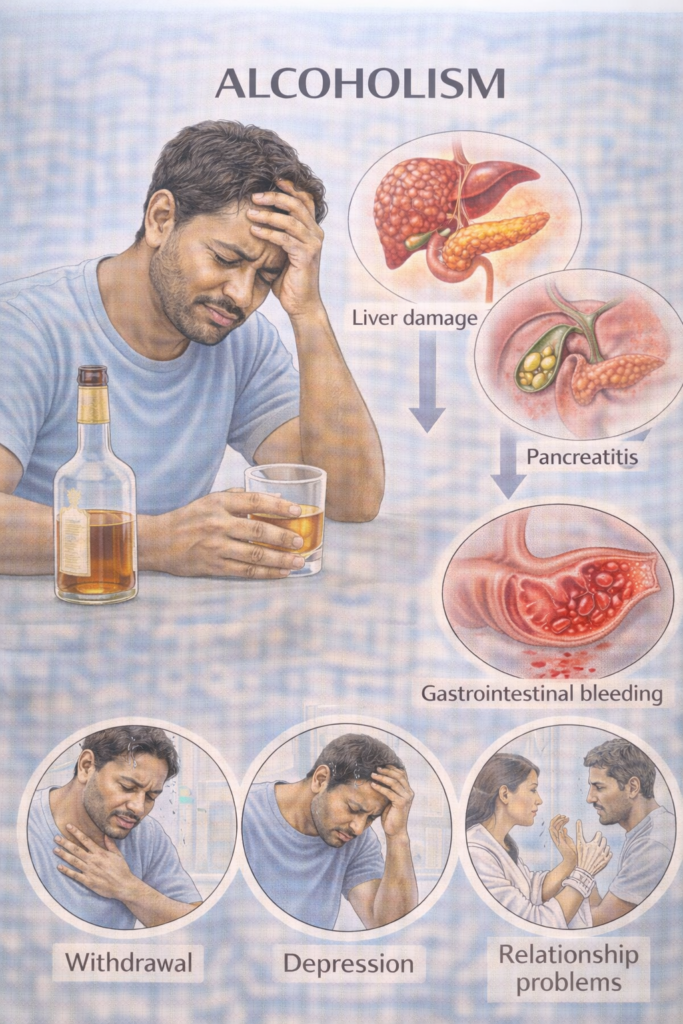
Tremor, sweating, agitation (withdrawal).
Jaundice, hepatomegaly, ascites (liver disease).
Peripheral neuropathy, Wernicke’s (thiamine deficiency).
Social/occupational impairment.
🔬 Investigations (Stepwise PARA Focus)
| Step | Investigation | Purpose |
|---|---|---|
| 1️⃣ Initial | FBC (macrocytosis, anaemia, thrombocytopenia) | Detect alcohol-related marrow/liver effects |
| LFTs (↑GGT, ↑AST>ALT, ↑bilirubin, ↓albumin) | Suggests alcoholic liver disease | |
| U&E, glucose, clotting (INR) | Assess systemic impact | |
| 2️⃣ Screening | AUDIT-C, CAGE | Identify hazardous drinking |
| 3️⃣ Imaging | USS liver | Fatty infiltration, cirrhosis |
| 4️⃣ Advanced | Fibroscan, liver biopsy | Stage fibrosis if indicated |
💊 Management (NICE CG115 / SIGN 74)
| Step | Intervention | Notes |
|---|---|---|
| 1️⃣ Acute withdrawal | Benzodiazepines (e.g. chlordiazepoxide) taper | Prevent delirium tremens/seizures |
| Thiamine (Pabrinex IV if malnourished; oral prophylaxis otherwise) | Prevent Wernicke’s | |
| 2️⃣ Relapse prevention | Acamprosate, naltrexone, disulfiram | Specialist initiation |
| 3️⃣ Supportive | Detox programmes, CBT, motivational interviewing | Community or inpatient |
| 4️⃣ Liver disease | Alcohol abstinence = only proven therapy | Consider transplant in end-stage cirrhosis |
| 5️⃣ Social support | AA, community alcohol services, safeguarding | Multidisciplinary input |
⚠️ Complications
Acute: Withdrawal seizures, delirium tremens, Wernicke’s encephalopathy.
Chronic: Cirrhosis, HCC, GI bleeding (varices), pancreatitis, cardiomyopathy, neuropathy, depression, suicide.
📅 Follow-up
Monitor abstinence: LFTs, CDT/PEth testing if needed.
GP / alcohol services follow-up.
Screen for comorbidities: depression, malnutrition, liver cancer (US + AFP if cirrhotic).
Long-term relapse prevention programmes.
🔎 Key PARA Exam Traps
AST > ALT (usually ratio >2:1) = alcoholic liver disease.
Always give thiamine before glucose in suspected Wernicke’s.
Alcohol withdrawal = benzodiazepines (not antipsychotics).
Acamprosate/naltrexone = relapse prevention; disulfiram rarely first-line.
Do not “treat” asymptomatic raised GGT with drugs → investigate alcohol use.


- PARA-aligned, reviewed February 2026
Educational platform. Not medical advice.
