14. Disorders of the Gallbladder & Biliary Tract
(aligned to GMC PARA map — gallbladder is listed, biliary tract folded in for clinical completeness)
 Definition
Definition
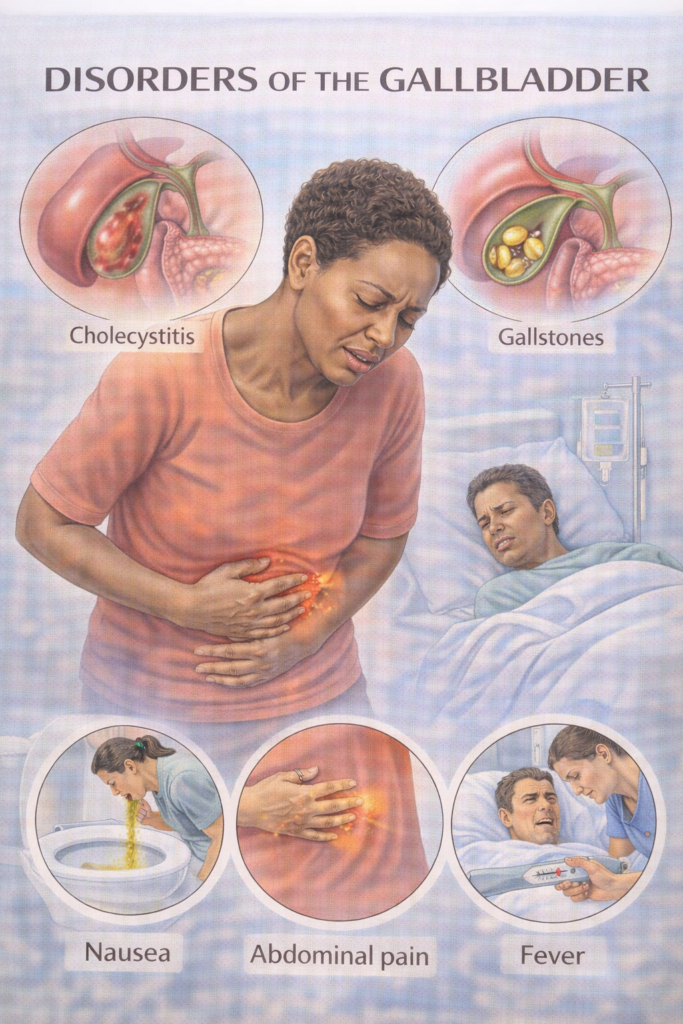
A spectrum of conditions affecting the gallbladder and biliary tract, most caused by gallstones (cholelithiasis) → may lead to pain, infection, obstruction, jaundice, or pancreatitis.
Gallstone types:
Cholesterol (80%, linked to 5Fs).
Pigment (black/brown; haemolysis, infection).
Mixed (commonest in practice).
 Risk Factors “5 Fs” classic
Risk Factors “5 Fs” classic
Female, Forty, Fat, Fertile, Fair (Caucasian).
↑ Risk in South Asians (higher pigment stone prevalence in UK).
Other: haemolysis (pigment stones), rapid weight loss, diabetes, pregnancy, Crohn’s (ileal disease).
🔬 Pathophysiology of Gallbladder Disorders
| Disorder | Pathophysiology |
|---|---|
| Biliary colic | Gallstone transiently obstructs cystic duct → ↑ pressure → visceral pain. No infection. |
| Acute cholecystitis | Persistent cystic duct obstruction → bile stasis → bacterial infection (E. coli, Klebsiella, Enterococcus) → inflammation + oedema. |
| Empyema | Untreated acute cholecystitis → pus in lumen → high risk sepsis → surgical emergency. |
| Chronic cholecystitis | Recurrent inflammation → fibrosis + shrunken gallbladder → dysmotility → ↑ gallbladder cancer risk. |
| Gallstone ileus | Large stone erodes wall → cholecysto-enteric fistula → stone enters bowel → SBO (terminal ileum). |
| Gallbladder cancer | Chronic inflammation (stones, porcelain GB) → dysplasia → adenocarcinoma. Poor prognosis. |
 Core Gallbladder Conditions
Core Gallbladder Conditions
| Disorder | Key Features | Exam Traps |
|---|---|---|
| Biliary colic | RUQ/epigastric pain (episodic, after fatty meals), radiates to scapula, no fever/jaundice. | Pain not truly colicky — constant. Bloods normal. |
| Acute cholecystitis | RUQ pain + fever, Murphy’s sign +, raised WCC/CRP. | USS: wall thickening + pericholecystic fluid. |
| Empyema of GB | Pus-filled gallbladder, septic patient. | Needs urgent IV abx + drainage. |
| Chronic cholecystitis | Recurrent low-grade RUQ pain, fibrosis. | Follows repeated acute attacks. |
| Gallstone ileus | Small Bowel Obstruction (SBO) from stone via fistula. Elderly women. | Rigler’s triad on AXR/CT: SBO + pneumobilia + ectopic stone. |
| Gallbladder cancer | Rare, linked to chronic stones/porcelain GB. | Poor prognosis, often incidental. |
📄 Jaundice Framework — Pre-hepatic, Hepatic, Post-hepatic
| Type | Pathophysiology | Key Features | Typical Causes | Test Clues |
|---|---|---|---|---|
| Pre-hepatic | ↑ Haemolysis → excess unconjugated bilirubin exceeds liver conjugation capacity | Mild jaundice, no bilirubinuria, dark stools | Haemolysis (AIHA, sickle cell, G6PD, malaria) | ↑ unconjugated bilirubin, normal LFTs, anaemia, ↑ retics |
| Hepatic | Hepatocellular injury or impaired conjugation/excretion → mixed hyperbilirubinaemia | Jaundice ± systemic illness, CLD stigmata | Viral hepatitis, ALD, MASLD, cirrhosis, drugs | ↑ ALT/AST > ALP, deranged INR/albumin |
| Post-hepatic (obstructive) | Blocked bile ducts → conjugated bilirubin refluxes into blood | Dark urine, pale stools, pruritus, RUQ pain | Gallstones, strictures, cholangiocarcinoma, pancreatic cancer | ↑ conjugated bilirubin; ↑ ALP/GGT > ALT; duct dilatation on US/MRCP |
💡 Exam Hotspot – Gilbert’s Syndrome
Definition: Benign inherited ↓ UDP-glucuronyl transferase → impaired conjugation of bilirubin.
Features: Isolated unconjugated hyperbilirubinaemia; intermittent mild jaundice (triggered by fasting, illness, alcohol, stress).
Tests: Normal LFTs, no haemolysis, only ↑ unconjugated bilirubin.
Exam Trap: Don’t confuse with hepatic pathology — everything else is normal.
Management: Reassure — no treatment required.
- Placement note: Not a GMC PARA core condition, but very common in exam vignettes to test your jaundice framework knowledge.
🧠 Exam triggers:
Dark urine + pale stools + pruritus → obstructive/ post-hepatic
Normal LFTs + unconjugated bilirubin → pre-hepatic/ Guilbert’s (benign)
Stigmata of CLD → hepatic.
- Anaemia + ↑ reticulocytes + jaundice → pre-hepatic haemolysis.
📎 See also: “Liver Failure (including Cirrhosis)” for detailed intra-hepatic causes and management.
⚠️ Core Biliary Tract Conditions
| Disorder | Key Features | Exam Traps |
|---|---|---|
| Choledocholithiasis | Stone in common bile duct (CBD) → RUQ pain, cholestatic LFTs (↑ALP, ↑bilirubin). | USS may miss CBD stones → MRCP better. |
| Ascending cholangitis | Infection + obstruction → Charcot’s triad: RUQ pain, fever, jaundice. Reynolds’ pentad if + hypotension & confusion (sepsis). | Always needs IV abx + urgent biliary decompression (ERCP). |
| Obstructive jaundice | Painless jaundice (think malignancy: pancreatic/ampullary/CCA) vs painful (stones). | Courvoisier’s law: palpable, non-tender GB unlikely due to stones (think cancer). |
| Gallstone pancreatitis | Gallstone impacts ampulla → blocks bile + pancreatic ducts → acute pancreatitis (lipase > amylase). | Do not confuse with biliary colic/cholecystitis. USS first-line, MRCP for CBD stones. Cholecystectomy after recovery to prevent recurrence. |
🔬 Pathophysiology of Biliary Tract Disorders
| Disorder | Pathophysiology |
|---|---|
| Choledocholithiasis | Gallstone migrates from gallbladder → lodges in common bile duct (CBD) → obstruction of bile outflow → conjugated hyperbilirubinaemia, cholestatic LFTs. |
| Ascending cholangitis | Obstructed CBD becomes infected (E. coli, Klebsiella, Enterococcus) → ↑ pressure + bacterial proliferation → systemic sepsis. |
| Obstructive jaundice (stones/malignancy) | Bile cannot drain → conjugated bilirubin refluxes into blood → dark urine, pale stools, pruritus. Chronic obstruction → secondary biliary cirrhosis. |
| Gallstone pancreatitis | Stone at ampulla of Vater blocks both CBD + pancreatic duct → reflux/activation of pancreatic enzymes → acute pancreatitis. |
Choledocholithiasis = obstruction, no infection.
Cholangitis = obstruction + infection (Charcot’s triad ± Reynolds’ pentad).
Obstructive jaundice can be benign (stone, stricture) or malignant (pancreatic/ampullary/CCA).
Gallstone pancreatitis is a biliary complication but often tested under pancreas.
📦 Additional: Autoimmune Cholestatic Disorders (Not PARA Core, but Exam-Linked)
| Feature | Primary Biliary Cholangitis (PBC) | Primary Sclerosing Cholangitis (PSC) |
|---|---|---|
| Who | Middle-aged women (F>M) | Young/middle-aged men (M>F), strong IBD (UC) link |
| Pathophysiology | Autoimmune destruction of intra-hepatic bile ducts | Inflammation + fibrosis of intra & extra-hepatic bile ducts (“onion-skin”) |
| Clinical | Pruritus, fatigue, jaundice; xanthelasma/xanthomas, osteoporosis | Fatigue, pruritus, jaundice; recurrent cholangitis; progression to cirrhosis |
| Antibody | AMA (anti-mitochondrial, 90–95%) | p-ANCA (non-specific) |
| LFTs | Cholestatic: ↑ALP, ↑GGT > ↑ALT/AST | Cholestatic: ↑ALP, ↑GGT; may be fluctuating |
| Complications | Cirrhosis, portal HTN, ↑ risk hepatocellular carcinoma | Cirrhosis, cholangiocarcinoma (10–15%), colorectal cancer (with UC) |
| Diagnosis | AMA + cholestatic LFTs ± liver biopsy | MRCP/ERCP: multifocal strictures + dilatations (“beading”) |
| Management | UDCA (ursodeoxycholic acid), symptom relief (cholestyramine for itch), liver transplant if end-stage | ERCP for dominant strictures, manage complications, liver transplant if end-stage |
🧠 Memory hook
PBC = AMA, intra-hepatic, women, xanthelasma
PSC = p-ANCA, beading ducts, men with UC, cholangiocarcinoma risk
 Investigations
Investigations
| Step | Investigation | Purpose |
|---|---|---|
 Initial Initial | Serum amylase or lipase (>3× ULN) | Diagnostic – lipase preferred (more sensitive/specific). |
| FBC, CRP, U&E, LFTs, glucose, calcium, ABG | Assess systemic impact, inflammation, severity. | |
 Imaging Imaging | USS abdomen (first-line) | Detect gallstones, gallbladder wall thickening, duct dilatation. |
| MRCP | Non-invasive biliary tree assessment – choledocholithiasis, obstruction. | |
| ERCP | Diagnostic + therapeutic (stone removal, stenting) – not first-line. | |
| CT abdomen (contrast) | If complications suspected (perforation, pancreatitis, ileus, cancer). | |
 Prognostic (if pancreatitis suspected) Prognostic (if pancreatitis suspected) | Glasgow-Imrie score, CRP >150, APACHE II | Predicts severity, guides HDU/ICU |
💊 Management (Stepwise – NICE / BSG)
| Condition | First-line | Escalation / Notes |
|---|---|---|
| Biliary colic | Analgesia (NSAIDs/opioids), lifestyle advice | Elective laparoscopic cholecystectomy if recurrent |
| Acute cholecystitis | Admit, IV fluids, analgesia, IV antibiotics (co-amoxiclav) | Laparoscopic cholecystectomy <1 week (ideally within 72 hrs) |
| Choledocholithiasis | ERCP stone extraction ± stent | Then laparoscopic cholecystectomy |
| Cholangitis | IV antibiotics (pip-taz or ceftriaxone + metronidazole), sepsis 6 | Urgent ERCP for biliary drainage |
| Gallbladder empyema | IV antibiotics + drainage | Surgical consult urgent |
| Gallbladder cancer | Staging CT, MDT discussion | Surgery ± palliative care |
📋 Follow-Up
Post-cholecystectomy: recovery usually complete; warn about occasional bile salt diarrhoea.
Gallstone pancreatitis: offer cholecystectomy during same admission.
Gallbladder cancer: oncology/hepatobiliary follow-up, often palliative.
PSC/PBC (if overlap suspected): hepatology monitoring.

Murphy’s sign = cholecystitis, not biliary colic.
Charcot’s triad ± Reynold’s pentad = cholangitis (sepsis, urgent ERCP).
ERCP = therapeutic, not just diagnostic.
Asymptomatic stones = no treatment unless porcelain GB, sickle cell, or very high risk.
Courvoisier’s law = malignancy > stones.
USS first-line, MRCP next for ductal stones, ERCP = therapeutic.
Biliary colic = pain only, normal bloods.
Acute cholecystitis = pain + fever + raised WCC/CRP.
Lipase > amylase for diagnosing gallstone pancreatitis.
📅 Last updated in line with NICE NG104 (Gallstone disease) & BSG Guidelines
Published: 2014 • Last updated: 2022
- PARA-aligned, reviewed February 2026
🔒 PASSMAP ensures all content is PARA-aligned, exam-focused, and NICE-compliant.
Educational platform. Not medical advice.
