12. Liver Failure (including Cirrhosis)
 Definition
Definition
Liver failure = loss of hepatic synthetic & detoxifying capacity → coagulopathy (INR ≥1.5), jaundice, ± encephalopathy.
Cirrhosis = end-stage diffuse hepatic fibrosis with nodular remodelling & portal hypertension; can be compensated or decompensated (ascites, variceal bleeding, jaundice, encephalopathy).
Acute liver failure (ALF) = INR ≥1.5 + any encephalopathy, no prior cirrhosis.
Acute-on-chronic liver failure (ACLF) = acute decompensation of cirrhosis with organ failure(s) & high short-term mortality.
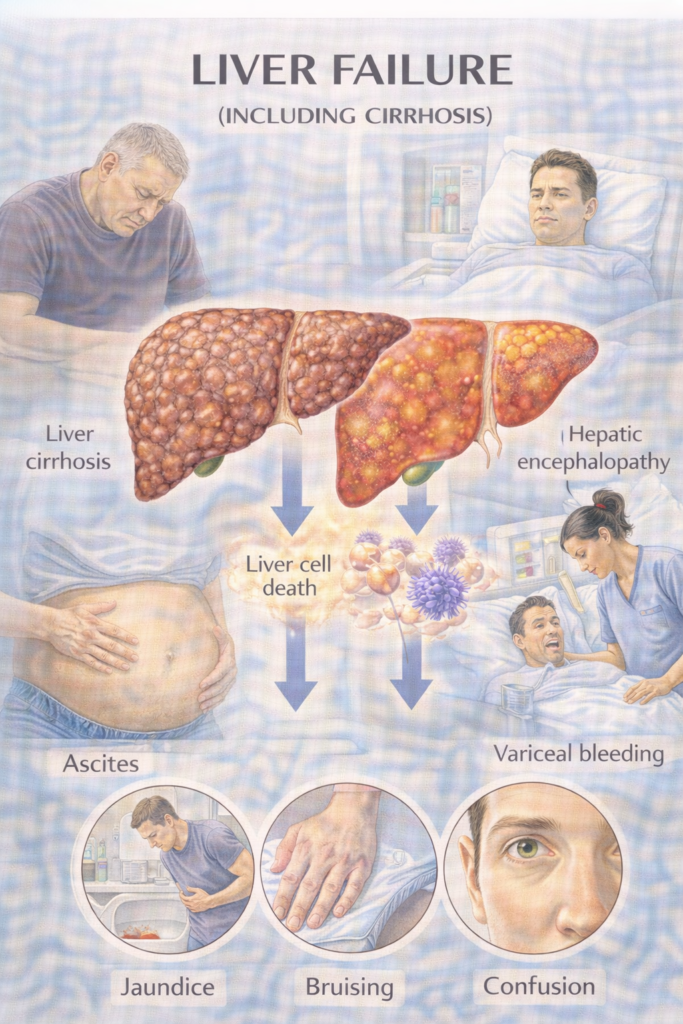
⚠️ Clinical Features of Cirrhosis / Liver Failure
| Category | Features | Exam Traps |
|---|---|---|
| General | Fatigue, weight loss, muscle wasting | Cachexia often overlooked in exam stems |
| Skin | Jaundice, spider naevi, palmar erythema, bruising | Think chronic vs acute (jaundice + coagulopathy = acute) |
| Abdomen | Ascites, splenomegaly, caput medusae | Splenomegaly = portal HTN |
| Endocrine | Gynaecomastia, testicular atrophy, amenorrhoea | Secondary to ↓ metabolism of sex hormones |
| Neuro | Hepatic encephalopathy (confusion → coma, asterixis) | Flapping tremor = classic |
| Decompensated | Ascites, variceal bleeding, encephalopathy, jaundice | “Decompensation = one of the 4” |
📄 Types of Jaundice — High-Yield Framework
🔬 Bilirubin Metabolism Explained
Production – Breakdown of haemoglobin → unconjugated bilirubin (water-insoluble).
Transport – Unconjugated bilirubin binds to albumin → delivered to liver.
Conjugation – Hepatocytes convert unconjugated → conjugated bilirubin via UGT enzyme (UDP-glucuronyltransferase). Conjugated = water-soluble.
Excretion – Conjugated bilirubin excreted into bile → intestine (converted to stercobilin in stool → brown colour; urobilin in urine → yellow colour).
Why it matters in exams
Unconjugated bilirubin ↑ = pre-hepatic causes (haemolysis, Gilbert’s).
Conjugated bilirubin ↑ = post-hepatic obstruction (stones, tumours, PSC, PBC).
Mixed pattern = hepatic dysfunction (viral hepatitis, cirrhosis, alcohol, drugs).
💡 Exam tip: Dark urine = conjugated hyperbilirubinaemia (water soluble → excreted in urine). Pale stools = obstructive jaundice (no stercobilin).
Helps separate differentials when jaundice is present.
| Type | Mechanism | Key Features | Causes (examples) |
|---|---|---|---|
| Pre-hepatic | ↑ Bilirubin production (unconjugated) | No dark urine (unconjugated not water-soluble), ± anaemia | Haemolysis, ineffective erythropoiesis |
| Hepatic | Impaired conjugation/processing | Mixed conjugated/unconjugated; ↑ ALT/AST; systemic illness | Viral hepatitis, alcohol, cirrhosis, Wilson’s, drugs (paracetamol, methotrexate) |
| Post-hepatic (obstructive) | Blocked bile outflow (conjugated) | Dark urine, pale stools, pruritus | Gallstones, pancreatic/pancreatobiliary cancer, cholangiocarcinoma, PSC, PBC, biliary atresia |
🧠 Memory hook:
Pre = Production problem
Hepatic = Handling problem
Post = Plumbing problem
 Aetiology / Risk (by jaundice category)
Aetiology / Risk (by jaundice category)
| Category | Examples (high-yield) | PARA Exam Traps |
|---|---|---|
| Pre-hepatic (before liver – ↑ unconjugated bilirubin) | Haemolysis: autoimmune haemolysis, sickle cell, thalassaemia, G6PD deficiency. Gilbert’s syndrome (benign ↓UGT activity). | Normal LFTs, ↑ unconjugated bilirubin, no bilirubinuria. Gilbert’s often triggered by stress/fasting. |
| Hepatic (intra-liver – impaired conjugation/excretion) | Alcohol: chronic harmful use, binge → decompensation. Viral: HBV, HCV (chronic), HAV/HEV (acute; HEV high risk in pregnancy). Metabolic: MASLD, haemochromatosis, Wilson’s disease, α-1 antitrypsin deficiency. Autoimmune/cholestatic: AIH, PBC, PSC. Vascular/Ischaemic: Budd–Chiari, shock liver. Drugs/Toxins: Paracetamol, valproate, isoniazid, methotrexate, amiodarone, alcohol. Other: Malignancy infiltration, pregnancy syndromes (AFLP, HELLP). | Mixed pattern on LFTs: ↑ ALT/AST ± ↑ bilirubin. Severe cases → prolonged INR/low albumin. |
| Post-hepatic (obstructive/cholestatic – ↑ conjugated bilirubin) | Gallstones (choledocholithiasis). Malignancy: pancreatic, ampullary, cholangiocarcinoma. Strictures, PSC. Parasites (rare in UK). | Dark urine, pale stools, pruritus. LFTs: ↑ALP, ↑GGT > transaminases. Courvoisier’s law: palpable, non-tender GB = malignancy. |
While the GMC PARA map lists “Liver failure (including cirrhosis)” as a single entity, in clinical practice and exams the underlying cause is often the key to diagnosis, prognosis and management.
Certain aetiologies are disproportionately represented in UK practice and exam stems because they carry distinctive clinical clues and require specific investigations or treatments.
These are the so-called High-Yield Liver Disorders — they include metabolic and autoimmune/cholestatic diseases (e.g. PBC, PSC, Wilson’s, Haemochromatosis, A1AT Deficiency).
Understanding them helps link the broad category of liver failure with the real-world diseases Physician Associates will encounter and be tested on.
📄 High-Yield Liver Aetiologies — Mini Definitions
Primary Biliary Cholangitis (PBC)
Chronic autoimmune destruction of intrahepatic bile ducts → progressive cholestasis and fibrosis. Strong female predominance.
Primary Sclerosing Cholangitis (PSC)
Progressive inflammation and fibrosis of intra + extrahepatic bile ducts → multifocal strictures and cholestasis. Strongly associated with ulcerative colitis and cholangiocarcinoma risk.
Wilson Disease
Autosomal recessive ATP7B mutation → defective copper metabolism → accumulation in liver, brain, cornea (Kayser–Fleischer rings). Presents <40 yrs.
Haemochromatosis
Autosomal recessive HFE mutation → ↑ intestinal iron absorption → iron overload in liver, pancreas, heart, joints. Classically middle-aged men.
Alpha-1 Antitrypsin Deficiency (A1ATD)
Inherited deficiency/misfolding of A1AT → hepatic accumulation (cirrhosis/HCC risk) + early panacinar emphysema (COPD phenotype in non-smokers).
📦 🔑 Exam Spotlight — High-Yield Liver Disorders
👉 Although “Liver Failure (including cirrhosis)” is the formal PARA heading, exam stems often test the cause of liver disease. These specific conditions appear frequently because they have:
Classic patient demographics (e.g. middle-aged woman with fatigue + pruritus → PBC)
Distinctive diagnostic clues (e.g. Kayser–Fleischer rings → Wilson disease)
Targeted first-line management (e.g. venesection in haemochromatosis)
✅ Memorise the following table — it compresses the aetiology screen into the 5 highest-yield disorders for exams and clinical practice.
 High-Yield Liver Disorders
High-Yield Liver Disorders
| Disorder | Typical Patient | Key Features | Diagnostic Clues | Management (1st-line / key) |
|---|---|---|---|---|
| PBC (Primary Biliary Cholangitis) | Middle-aged woman | Fatigue, pruritus, jaundice, xanthelasma | ↑ALP, +AMA (anti-mitochondrial antibody) | Ursodeoxycholic acid; transplant if end-stage |
| PSC (Primary Sclerosing Cholangitis) | Young/mid-aged man, IBD (esp. UC) | Fatigue, pruritus, jaundice | ↑ALP, p-ANCA; MRCP “beading” | Symptomatic Tx; stents; transplant definitive |
| Wilson’s Disease | Teen/young adult | Hepatitis/cirrhosis, neuro (tremor, dystonia, psych), Kayser–Fleischer rings | ↓Ceruloplasmin, ↑urinary copper | Chelation (penicillamine, trientine), zinc |
| Haemochromatosis | Middle-aged man | Bronze skin, diabetes, arthropathy, cirrhosis | ↑Ferritin, ↑TSAT; HFE mutation | Venesection (phlebotomy) |
| α-1 Antitrypsin Deficiency | Young adult | Cirrhosis + emphysema | ↓A1AT levels, PAS+ globules in hepatocytes | Supportive; transplant if severe |
📊 Prognostic Scores
| Score | Parameters | Use |
|---|---|---|
| Child–Pugh (A–C) | Bilirubin, Albumin, INR, Ascites, Encephalopathy | Cirrhosis severity / prognosis |
| MELD-Na | Bilirubin, INR, Creatinine, Sodium | Predicts 3-month mortality; transplant listing |
🚩 When to Refer / Admit
| Urgency | Triggers | Action |
|---|---|---|
| 🚑 Immediate (ED) | ALF (INR ≥1.5 + encephalopathy), massive GI bleed, septic shock, rapidly rising bilirubin/INR, HEV in pregnancy, severe hyperkalaemia | Resuscitate; urgent hepatology/ICU; early transplant-centre discussion. |
| ⚡ Urgent (same/next day) | New decompensation (ascites, jaundice, encephalopathy), AKI (acute kidney injury) on cirrhosis, suspected SBP (spontaneous bacterial peritonitis), HRS-AKI (hepatorenal syndrome–AKI) | Acute medical/hepatology review; day-case/AMU. |
| 📮 Routine | Stable cirrhosis for surveillance/optimisation; unexplained abnormal LFTs with risk factors | Hepatology clinic; fibrosis assessment. |
🔬 Investigations (build a positive, cause-led diagnosis)
| Test | Why / What to look for |
|---|---|
| LFTs (ALT/AST = alanine/aspartate aminotransferases; ALP; bilirubin), albumin, INR, FBC (full blood count), U&E (urea & electrolytes), CRP, glucose | Severity, synthetic function, infection, metabolic derangement. |
| Ultrasound liver ± Doppler | Morphology, portal vein patency, splenomegaly, screening for HCC (hepatocellular carcinoma). |
| Aetiology screen | HBsAg/HCV antibody ± RNA, autoimmune (ANA/SMA/LKM-1, IgG), ferritin/transferrin saturation, ceruloplasmin (young), α-1 antitrypsin; consider HEV IgM in acute. |
| Elastography (transient elastography/FibroScan) or FIB-4 | Non-invasive fibrosis staging (stable patients). |
| OGD (oesophagogastroduodenoscopy) | Variceal screening if cirrhosis. |
| Ascites: diagnostic paracentesis | Cell count (PMN ≥250/µL = SBP), culture, albumin (SAAG), protein. Tap all inpatients with ascites. |
| Scores | Child–Pugh (A–C); MELD-Na (transplant priority/mortality risk). |
🔎 Interpreting LFT Patterns (Practical Exam Tips)
| Pattern | Typical Findings | Key Causes | Exam Pearls |
|---|---|---|---|
| Hepatocellular (ALT/AST predominant) | ALT/AST ↑↑ (>10× ULN), ALP mildly ↑ | Viral hepatitis, drugs/toxins (paracetamol, isoniazid), ischaemia | ALT usually > AST (except in alcohol). Massive ALT/AST >1000 = viral, drugs, ischaemia. |
| Alcohol-related | AST > ALT, usually both <500 | Alcoholic hepatitis, cirrhosis | AST:ALT >2 = alcohol-related in ~70% cases. Exam classic. |
| Cholestatic (ALP/GGT predominant) | ALP ↑↑, GGT ↑, mild ↑ ALT/AST | Biliary obstruction (stones, cancer, PSC, PBC) | Dark urine + pale stools + pruritus → obstructive picture. |
| Mixed pattern | ALT/AST + ALP both ↑ | Drug-induced liver injury (DILI), infiltrative disease, sepsis | Don’t forget sepsis can cause cholestasis with mixed LFTs. |
| Isolated bilirubin | ↑ unconjugated bilirubin only | Gilbert’s, haemolysis | Normal ALT/ALP; benign in Gilbert’s. |
💡 Exam Triggers
AST:ALT >2 = alcohol-related (MCQ favourite).
ALT >1000 = think viral, paracetamol, ischaemic hepatitis.
ALP > ALT/AST = cholestatic → biliary obstruction (gallstones, PSC, cancer).
Gilbert’s = isolated unconjugated bilirubin, normal other LFTs.
 Management
Management
A) Acute Liver Failure (ALF)
What it is: sudden loss of hepatic function without prior cirrhosis; classic hallmark = INR (international normalised ratio) ≥1.5 + any encephalopathy.
Why dangerous: cerebral oedema, coagulopathy, sepsis → high short-term mortality
| Step | What to do |
|---|---|
| A–B–C | Airway (consider intubation if encephalopathy), Breathing, Circulation; escalate early to ICU/LTU (liver transplant unit). |
| N-acetylcysteine (NAC) | Give immediately in paracetamol ALF; consider in non-paracetamol ALF (benefit on transplant-free survival). |
| Monitor/replace | Hourly neuro obs; prevent hypoglycaemia (glucose infusion); correct K⁺/Mg²⁺/PO₄³⁻; manage coagulopathy only for procedures. |
| Infection | Culture blood/urine/ascites; treat sepsis early (broad-spectrum per local policy). |
| Avoid | Sedatives, unnecessary protein restriction, hepatotoxins; specialist management of raised ICP. |
| Transplant | Apply prognostic criteria (e.g., King’s concepts) and discuss listing early. |
B) Decompensated Cirrhosis
Why dangerous: each complication can rapidly precipitate multi-organ failure; always search for triggers (sepsis, GI bleed, alcohol/drugs, constipation, dehydration, electrolytes).
1) Ascites
What: pathological peritoneal fluid due to portal hypertension and sodium/water retention.
Why dangerous: SBP (spontaneous bacterial peritonitis), HRS-AKI (hepatorenal syndrome–acute kidney injury), malnutrition/respiratory compromise.
| Step | Treatment | Key notes |
|---|---|---|
| Initial | Alcohol stop; no NSAIDs; moderate salt restriction | Avoid very low protein diets. |
| Diuretics | Spironolactone up-titrate (e.g., 100 mg) ± furosemide (e.g., 40 mg) keeping 100:40 mg ratio | Target weight change 0.5 kg/day (no oedema) or 1 kg/day (with oedema). |
| LVP — Large-Volume Paracentesis | Remove >5 L ascites with albumin | Albumin ~8 g per L removed. |
| Refractory | Consider TIPS (transjugular intrahepatic portosystemic shunt) if suitable | Otherwise serial LVP + albumin. |
| Prophylaxis | Low ascitic protein (<15 g/L) or prior SBP → antibiotic prophylaxis | Follow local policy. |
2) SBP — Spontaneous Bacterial Peritonitis
What: infection of ascitic fluid without an obvious source.
Why dangerous: sepsis, renal failure, death if missed.
| Diagnosis | PMN ≥250/µL in ascitic fluid = treat now |
|---|---|
| Antibiotics | IV 3rd-gen cephalosporin (e.g., cefotaxime/ceftriaxone) then tailor to culture |
| Albumin | Day 1: 1.5 g/kg • Day 3: 1 g/kg (reduces renal failure/mortality) |
| Secondary prophylaxis | Long-term oral agent (e.g., quinolone) per local protocol |
3) Variceal Haemorrhage
What: bleeding from oesophageal/gastric varices due to portal hypertension.
Why dangerous: exsanguination, aspiration, encephalopathy.
| Immediate | Restrictive transfusion (Hb target ~70–80 g/L), terlipressin IV, prophylactic antibiotics (e.g., ceftriaxone) |
|---|---|
| Endoscopy | Urgent band ligation (EVL). If uncontrolled → balloon tamponade bridge; consider early TIPS in high-risk. |
| Secondary prevention | NSBB — Non-selective β-blocker (propranolol/carvedilol) + repeat EVL to eradication. |
| Primary prevention | For medium/large varices: NSBB or EVL if β-blocker contraindicated. |
4) Hepatic Encephalopathy (HE)
What: brain dysfunction from ammonia/toxins + precipitants (sepsis, bleed, constipation, electrolyte imbalance).
Why dangerous: airway risk, poor adherence, recurrent admissions.
| Precipitants | Sepsis, GI bleed, constipation, electrolyte imbalance, dehydration, sedatives |
|---|---|
| Treatment | Lactulose titrated to 2–3 soft stools/day; add rifaximin for recurrent HE or poor control; correct triggers; avoid sedatives |
5) HRS-AKI — Hepatorenal Syndrome (acute kidney injury)
What: functional renal failure in advanced cirrhosis due to extreme splanchnic vasodilation/renal vasoconstriction.
Why dangerous: rapid renal decline; mortality without reversal.
| Diagnosis | Cirrhosis + AKI not responding after diuretic stop and albumin 1 g/kg day 1 then day 2, with no shock/nephrotoxins/structural kidney disease |
|---|---|
| Treatment | Terlipressin + albumin; treat sepsis; consider TIPS in select cases; renal replacement as bridge; early transplant referral |
6) Hyponatraemia
What: dilutional fall in sodium from water retention (vasopressin excess) in cirrhosis.
Why dangerous: seizures if severe/rapid shifts; worsens encephalopathy.
| Principle | Fluid restrict if severe/symptomatic; stop offending drugs; slow correction (avoid osmotic demyelination). |
7) Nutrition
What: catabolic state with muscle loss and micronutrient deficiency.
Why dangerous: infections, falls, poor wound-healing, worse outcomes.
| Goals | 1.2–1.5 g/kg/day protein, frequent meals + late-evening snack; add vitamin D, zinc if low; no routine protein restriction once HE controlled; dietitian early. |
C) Chronic Cirrhosis — Clinic Bundle
What it is: long-term care to slow disease, prevent complications, and spot cancer early.
Why it matters: reduces admissions and mortality; identifies transplant candidates in time.
| Bundle | What to do |
|---|---|
| Aetiology therapy | Alcohol cessation; antivirals for HBV/HCV; immunosuppression for AIH; manage MASLD (weight, diabetes, lipids). |
| Varices | OGD screening; NSBB or EVL when indicated; educate re bleed signs. |
| Vaccines | HAV/HBV; influenza; pneumococcal as per local schedule. |
| HCC surveillance | Ultrasound ± AFP (alpha-fetoprotein) every 6 months for all cirrhosis. |
| Medicines review | Avoid NSAIDs; review ACEi/ARB/diuretics in AKI; PPI only if indicated (infection risk). |
| Transplant | Refer early if MELD-Na rising, refractory ascites, recurrent HE, recurrent variceal bleeding, or poor quality of life. |
| Supportive care | Frailty/bone health, falls prevention, nutrition, goals/ceilings of care discussion. |
📅 Last updated in line with — 12. Liver Failure (including Cirrhosis)
NICE NG50 — Cirrhosis in over 16s: assessment & management. Published: 6 Jul 2016 • Last updated: 8 Sep 2023. Core UK guidance for assessment, surveillance (e.g., ultrasound ± AFP every 6 months), and prevention/early management of complications. NICE+1
NICE CG141 — Acute upper gastrointestinal bleeding (includes variceal care). Published: 13 Jun 2012 • Last reviewed: 29 Nov 2018 (no update required at that review). Supports restrictive transfusion and urgent endoscopy pathways. NICEPMC
NICE NG24 — Blood transfusion (cross-referenced for UGIB thresholds). Published: 18 Nov 2015; recommendations reference the acute UGIB guideline for resuscitation/anticoagulant reversal. NICE
NICE QS152 — Liver disease (quality standard). Priority areas for improving identification, fibrosis assessment, and cirrhosis care. NICE
- PARA-aligned, reviewed February 2026
Educational platform. Not medical advice.
