11. Hepatitis (viral, autoimmune)
 Definition
Definition
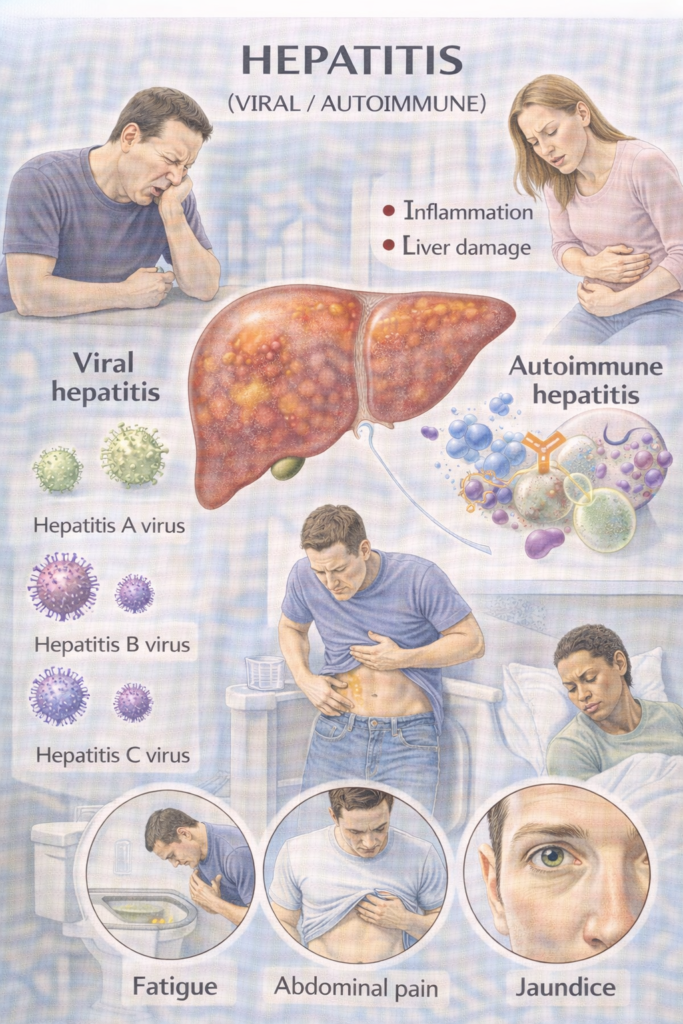
Hepatitis = inflammation of the liver, usually shown by raised ALT/AST with or without jaundice.
Hepatitis A virus (HAV) and Hepatitis E virus (HEV): typically acute, self-limited (faeco-oral).
Hepatitis B virus (HBV) and Hepatitis C virus (HCV): blood-borne; can become chronic and lead to cirrhosis/HCC.
HDV (Hepatitis D virus): a defective virus that depends on HBV. It uses the Hepatitis B surface antigen (HBsAg) to enter cells and assemble
Therefore HDV occurs only with HBV—as coinfection (catch both together) or superinfection (HDV added to chronic HBV). Memory line: “No HBsAg, no HDV.”
Autoimmune (AIH): immune-mediated hepatocellular inflammation (often IgG↑, ANA/SMA/LKM-1 positive) that responds to steroids.
 Aetiology / Risk Factors
Aetiology / Risk Factors
-
Viral: travel (HAV/HEV), blood/sex/vertical transmission (HBV/HCV), pork/wild game (HEV), HDV only in HBsAg-positive people.
-
Autoimmune: female sex, other autoimmune disease, drug-triggered AIH-like patterns.
-
General: alcohol, metabolic dysfunction-associated steatohepatitis, drugs/toxins.
 Clinical Features
Clinical Features
Acute viral hepatitis: malaise, anorexia, RUQ pain, dark urine, pale stools, jaundice; ALT/AST often very high.
Chronic hepatitis (HBV/HCV/AIH): often asymptomatic → fatigue, abnormal LFTs; later cirrhosis (ascites/varices) or HCC (hepatocellular carcinoma).
Extra-hepatic: HCV—cryoglobulinaemia, renal disease; HBV—polyarteritis nodosa; AIH—arthralgia/thyroid disease.
🧭 When to Refer — Red Flags & Pathways
| Tier | Triggers (examples) | Action |
|---|---|---|
| 🚑 Immediate emergency | Acute liver failure (coagulopathy and encephalopathy), severe sepsis, uncontrolled GI bleed, rapidly worsening jaundice; HEV in pregnancy | ED/acute take; urgent hepatology |
| ⚡ Urgent hepatology/gastro | Marked jaundice + rising INR, suspected AIH, decompensated cirrhosis, new HBsAg+ or HCV RNA+ with symptoms or fibrosis, suspected HDV | Fast-track clinic; specialist pathway |
| 📮 Routine | Newly diagnosed chronic HBV/HCV without instability; stable AIH for optimisation; vaccine/PEP questions | Viral hepatitis/AIH service |
HCC surveillance: 6-monthly ultrasound (± AFP) for all cirrhosis and for chronic HBV with significant fibrosis/cirrhosis.
🔬 Investigations in Hepatitis (Core Panels)
| Scenario | First-Line Tests | Confirmatory / Staging Tests | Key Notes for PARA |
|---|---|---|---|
| Suspected Acute Hepatitis | • LFTs (↑ ALT/AST) • FBC, U&E, INR, glucose • Pregnancy test (if relevant) • Viral screen: HAV IgM, HBsAg, anti-HBc IgM, HEV IgM, HCV Ab | • HCV RNA (if Ab +) • HEV RNA (if immunosuppressed) • Abdominal US (exclude obstruction, fatty liver) • Toxicology/drug screen | ⚠️ Always check INR + glucose early — acute liver failure risk. |
| Chronic HBV Screen | • HBsAg (screening) | If HBsAg+: • HBeAg, anti-HBe • HBV DNA PCR • ALT trend • Fibrosis staging: FIB-4, elastography • Always test: HDV (anti-HDV ± RNA), HIV | 🧠 HBsAg persisting >6 months = chronic infection. |
| Chronic HCV Screen | • HCV Ab (screening) | If Ab+: • HCV RNA PCR (confirms active infection) • Fibrosis staging (FIB-4, elastography) | 🧠 Treat all unless contraindicated — high PARA exam pearl. |
| Autoimmune Hepatitis (AIH) | • ALT/AST (hepatitic pattern) • ↑ IgG • ANA, SMA, LKM-1 Ab • Exclude viral hepatitis | • Liver biopsy (confirm diagnosis + subtype) • Apply Simplified AIH criteria • Monitor IgG/ALT for disease activity | ⚠️ PARA MCQ: Young female + ↑ IgG + ANA/SMA positivity → AIH. |
🧪 Hepatitis B Serology Interpretation
| HBsAg | Anti-HBs | Anti-HBc IgM | Anti-HBc IgG | Interpretation |
|---|---|---|---|---|
| – | – | – | – | Susceptible (never exposed, not immune) |
| – | + | – | – | Immune (Vaccination) |
| – | + | – | + | Immune (Past infection, resolved) |
| + | – | + | – / + | Acute infection (IgM confirms acute) |
| + | – | – | + | Chronic infection |
| – | – | – | + | “Isolated core antibody” → Could be: • Remote past infection (waning Anti-HBs) • False positive • Window period of acute infection |
🧪 Key Serology Interpretation (Exam-Focus)
HBsAg = infection (acute or chronic).
Anti-HBc IgM = acute infection.
Anti-HBc IgG = past or chronic infection.
Anti-HBs = immunity (vaccination or resolved infection).
Chronic = HBsAg positive >6 months.
🔑 PARA MCQ Traps
Acute hepatitis with encephalopathy + INR >1.5 → acute liver failure (admit/ITU).
Always biopsy gastric ulcers (exclude malignancy) BUT not duodenal ulcers.
In hepatitis B, isolated Anti-HBc IgG → think window period / past infection / false positive.
Treat chronic HCV regardless of fibrosis stage.
 Management
Management
A) Hepatitis A (HAV)
| Goal | Steps |
|---|---|
| Support | Fluids, rest, avoid alcohol/hepatotoxins; symptom control |
| Public health | Notify per local policy if indicated |
| PEP (post-exposure prophylaxis) | HAV vaccine for close contacts; consider human immunoglobulin for specific high-risk or vaccine-unsuitable contacts |
B) Hepatitis B (HBV)
| Scenario | What to do | Drugs | Monitoring / Notes |
|---|---|---|---|
| Acute HBV | Supportive; involve specialist if severe or acute liver failure | — | Watch INR, bilirubin, encephalopathy |
| Chronic HBV – who to treat | Treat if HBV DNA high with ALT elevation and/or significant fibrosis/cirrhosis (HBeAg status guides); treat all decompensated | Tenofovir (TDF or TAF) or entecavir; consider pegylated interferon in selected cases | ALT, HBV DNA, HBeAg/anti-HBe/HBsAg; renal/bone profile if on tenofovir; ultrasound ± AFP q6m if fibrosis/cirrhosis; test & vaccinate contacts; perinatal: neonatal schedule including birth dose |
C) Hepatitis C (HCV)
| Principle | Regimens | Before/during | Outcome |
|---|---|---|---|
| Treat all chronic HCV unless clear contraindication | DAAs (direct-acting antivirals) 8–12 weeks: e.g., sofosbuvir/velpatasvir or glecaprevir/pibrentasvir | Check HBsAg/anti-HBc (rare HBV reactivation); vaccinate HAV/HBV if non-immune; continue HCC surveillance if cirrhosis | >90–95% cure (SVR12 = sustained virologic response at 12 weeks) |
D) Hepatitis D (HDV)
| Who to test | Confirm | Treatment (specialist-led) | Prevention |
|---|---|---|---|
| All HBsAg-positive patients | Anti-HDV, then HDV RNA if positive | Options include bulevirtide in chronic HDV (centre-based) or pegylated interferon in selected cases | HBV vaccination prevents HDV (no HBsAg → no HDV) |
E) Hepatitis E (HEV)
| Population | What to do |
|---|---|
| Immunocompetent | Supportive care; avoid hepatotoxins |
| Pregnancy | Manage urgently with specialist input (higher severity) |
| Immunosuppressed / chronic HEV | Reduce immunosuppression if feasible; ribavirin course commonly used |
F) Autoimmune Hepatitis (AIH)
| Phase | Regimen | Targets & safety |
|---|---|---|
| Induction | Prednisolone ~0.5–1 mg/kg/day ± azathioprine (check TPMT—thiopurine methyltransferase—before starting) | Aim normal ALT/AST & IgG; counsel re side-effects |
| Maintenance | Taper steroids to lowest effective; continue azathioprine (or mycophenolate if intolerant) | FBC/LFTs for thiopurine toxicity; relapse is common—educate and plan |
 Prevention & PEP
Prevention & PEP
| Vaccine / PEP | Who | What |
|---|---|---|
| HBV vaccination | At-risk adults; routine childhood schedules; infants of HBsAg-positive mothers | Primary course (includes birth dose for exposed infants); some programmes include an extra hexavalent dose at ~18 months |
| HBV PEP | Significant exposure (needlestick, sexual, perinatal) | HBV vaccine ± HBIG according to timing/source status |
| HAV vaccination | Risk groups, travellers, outbreaks | Pre-exposure vaccine; PEP for close contacts |
🔁 Follow-Up & Monitoring
| Condition | Frequency | What to check | Escalate if… |
|---|---|---|---|
| Chronic HBV | Every 3–6 months | ALT, HBV DNA, HBeAg/HBsAg; renal/bone if on tenofovir; ultrasound ± AFP q6m if fibrosis/cirrhosis | Rising ALT/viral load, decompensation, pregnancy planning |
| Chronic HCV | Baseline → on-treatment → SVR12 at 12 weeks post-therapy | RNA result, adherence, drug interactions; continue HCC surveillance if cirrhosis | RNA detectable at end/12 weeks, LFT rise, decompensation |
| AIH | 2–4 weekly during induction → 1–3 monthly when stable | LFTs/IgG, FBC/LFTs for azathioprine safety | No biochemical response, toxicity, relapse |
🧠 Memory Box (fast recall)
| Tile | Meaning |
|---|---|
| “A & E = Acute & Enteric” | HAV/HEV are faeco-oral and usually acute |
| “B & C = Blood & Chronic” | HBV/HCV are blood-borne with chronicity risk |
| “No HBsAg, no HDV.” | HDV requires HBV surface antigen to exist |
| HBV serology — “S-C-E” | HBsAg = infection; anti-HBc IgM = acute; HBeAg = high infectivity; anti-HBs = immunity |
| Red-flag line | INR ≥1.5 + encephalopathy = acute liver failure → admit now |
| HCV in one line | DAAs for 8–12 weeks → >90–95% cure (SVR12) |
| AIH recipe | Prednisolone induction → azathioprine maintenance; check TPMT; aim normal ALT/IgG |
📅 Last updated in line with — Hepatitis (viral, autoimmune)
NICE CG165 — Hepatitis B (chronic): diagnosis & management. Published: 26 Jun 2013 • Last updated: 20 Oct 2017. NICE+1
NICE TA430 & TA507 — Direct-acting antivirals for HCV. TA430 (Sofosbuvir–Velpatasvir, 2017); TA507 (Sofosbuvir–Velpatasvir–Voxilaprevir, 2018). NICE+1
NICE TA896 — Bulevirtide for chronic HDV. Published: 07 Jun 2023. NICE
UKHSA Green Book, Chapter 18 (Hepatitis B) & UK schedule update. Chapter updated 2025; routine schedule adds 18-month hexavalent dose from 1 Jul 2025. GOV.UKGOV.UK+1
UKHSA Hepatitis E guidance. Collection last updated: 06 Jan 2025 (pregnancy severity; chronic HEV in immunosuppressed). GOV.UK
BSG Autoimmune Hepatitis guideline. New comprehensive update (2025) covering diagnosis, induction/maintenance therapy. Gutbsg.org.uk
- PARA-aligned, reviewed February 2026
Educational platform. Not medical advice.
