10. Haemorrhoids
 Definition
Definition
Dilated vascular cushions in the anal canal causing bleeding, prolapse, pain/itch, and lumps.
Internal haemorrhoids arise above the dentate line; external are below it.
 Aetiology
Aetiology
| Risk Factors | Examples |
|---|---|
| Raised intra-abdominal pressure | Constipation/straining, prolonged sitting, heavy lifting, chronic cough |
| Lifestyle & diet | Low fibre, dehydration |
| Physiological | Pregnancy/post-partum, ageing (support tissue laxity) |
| Medical | Anticoagulants/antiplatelets (apparent bleed ↑), portal hypertension (concurrent anorectal varices—separate entity) |
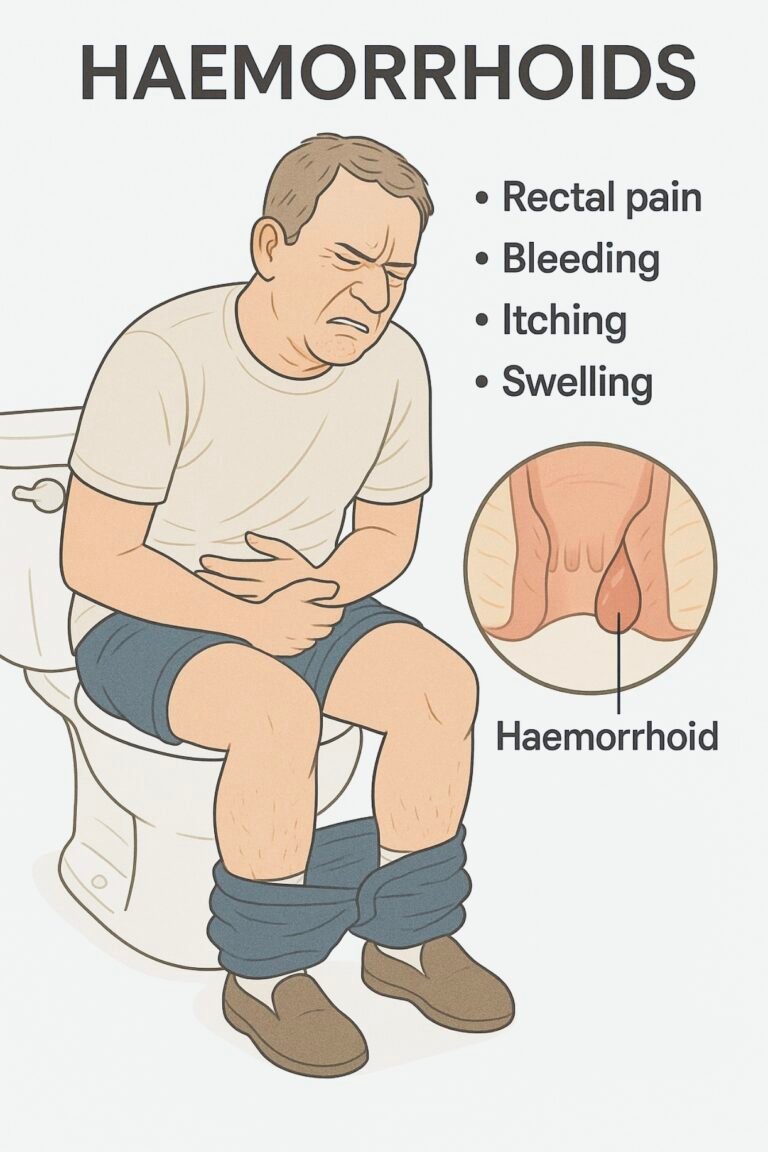
 Clinical Features
Clinical Features
| Symptom/sign | Typical of |
|---|---|
| Bright red rectal bleeding (on paper/bowl) | Internal > external |
| Prolapse ± mucus/soiling | Internal (grade II–IV) |
| Pruritus ani / irritation | Moisture/mucus |
| Painful perianal lump | Thrombosed external haemorrhoid |
| Exam | Inspection, DRE (digital rectal examination), proctoscopy if trained |
🧭 When to Refer — Red Flags & Pathways
| Tier | Key triggers (examples) | Action |
|---|---|---|
| 🚑 Immediate emergency | Haemodynamic instability, severe rectal pain with fever (abscess), brisk ongoing bleed | Same-day ED/acute surgical team |
| ⚡ Urgent suspected cancer – “2WW” | FIT (faecal immunochemical test) ≥10 µg Hb/g or NICE NG12 criteria (e.g., age ≥50 with unexplained rectal bleeding; ≥40 with unexplained weight loss + abdo pain; ≥60 with change in bowel habit or IDA – iron-deficiency anaemia) | CRC (colorectal cancer) 2-week-wait pathway; do not delay if clinical suspicion is high. |
| ⚡ Urgent colorectal | Acutely thrombosed external haemorrhoid within 72 h; incarcerated/prolapsed, oedematous internal piles; perianal sepsis | Consider excision/reduction; urgent clinic/ED per pain severity. |
| 📮 Routine | Persistent symptoms despite primary-care measures; recurrent bleeding without red flags | Colorectal clinic for office therapy |
Exam tip: Do not attribute bleeding to haemorrhoids until malignancy has been reasonably excluded (history, exam ± FIT/age-appropriate lower GI work-up).
🔎 Classification — Goligher (internal haemorrhoids)
| Grade | Description | Simple memory |
|---|---|---|
| I | Bleed; no prolapse | I = “Intraluminal only” |
| II | Prolapse on strain, spontaneously reduce | II = “In–out–back by itself” |
| III | Prolapse, manual reduction needed | III = “Hand helps” |
| IV | Irreducible prolapse ± strangulation | IV = “Fixed out” |
(Goligher classification.)
🔬 Investigations (primary care)
Clinical diagnosis after history + exam (inspection/DRE); proctoscopy if trained.
FBC if heavy/recurrent bleeding; consider FIT when CRC risk features present (per DG56/NG12). Routine colonoscopy not needed unless red flags.
 Management — (adults)
Management — (adults)
1) Foundations for all grades
| Measure | Detail |
|---|---|
| Fibre & fluids | Aim ~20–30 g/day fibre; maintain hydration |
| Stool softening | Macrogol/PEG (polyethylene glycol) first-line; avoid straining |
| Toilet habits | Short sits, respond to urge, avoid reading/phone time |
| Local care | Warm baths, gentle hygiene; short course topical local anaesthetic ± mild steroid for itch/pain (≤7 days) |
2) Office procedures (internal, persistent symptoms)
| Procedure | Indication | Notes |
|---|---|---|
| RBL (Rubber Band Ligation) | Grade II (and some I/III) | First-line; 1–3 bands/session; transient pain/bleed possible |
| Injection sclerotherapy | Grade I–II | Alternative if RBL unsuitable |
| Infrared coagulation | Grade I–II | Similar efficacy for small piles |
3) Surgical options (refractory/advanced)
| Operation | Indication | Notes |
|---|---|---|
| Excisional haemorrhoidectomy | Large grade III–IV or failed office therapy | Most durable; more post-op pain/time off work |
| Stapled haemorrhoidopexy (PPH) | Circumferential prolapsing internal haemorrhoids | Less pain, higher recurrence in some series |
| HAL/THD (Haemorrhoidal Artery Ligation ± Doppler / Transanal Haemorrhoidal Dearterialisation) | Selected grade II–IV | Lower pain; recurrence risk varies by centre |
4) Thrombosed external haemorrhoid
| Timeframe | Management |
|---|---|
| ≤48–72 h of onset | Consider excision under local anaesthetic for severe pain |
| >72 h or mild pain | Conservative (analgesia, stool softening, ice/sitz baths); review if worsening |
🔁 Follow-Up & Monitoring
| Phase | When | Check | Escalate if… |
|---|---|---|---|
| After foundations | 4–6 weeks | Bleeding, prolapse, pain/itch; stool form (Bristol); laxative use | Ongoing bleeding/prolapse → offer office therapy |
| After office therapy | 6–8 weeks | Symptom resolution; complications (pain/ulcer) | Persistent grade II–III → repeat office therapy or list for surgery |
| Post-surgery | Per local pathway | Wound/pain control, continence, return to activity | Secondary haemorrhage, fever, urinary retention → urgent review |
 Memory Boxes
Memory Boxes
Grades “B-S-M-I” → Bleed (I) • Self-reduce (II) • Manual (III) • Irreducible (IV). (Goligher)
First things first: FIBRE → Fibre/Fluids • Ignore straining • Brief time on loo • Regular activity • Emollient/short topicals. (CKS)
Office go-to: RBL for Grade II; I–II can also do sclerotherapy/infrared.
72-hour rule: Thrombosed external → consider excision ≤72 h if severe pain.
Don’t miss CRC: FIT ≥10 µg Hb/g or NG12 red flags → 2WW referral.
📅 Last updated in line with
NICE CKS — Haemorrhoids (primary-care diagnosis/management; office procedures overview). NICE
NICE DG56 (FIT to guide suspected CRC referral: threshold ≥10 µg Hb/g). NICE
NICE NG12 (Suspected cancer: recognition & referral—criteria including age ≥50 + rectal bleeding). NCBI
NICE TA128 (Stapled haemorrhoidopexy); NICE IPG on electrotherapy/HAL/THD for selected grades. NICE+1
- PARA-aligned, reviewed February 2026
Educational platform. Not medical advice.
