1. Pulmonary Hypertension
 Definition
Definition
Pulmonary hypertension (PH) is raised pressure in the pulmonary arterial system, defined as:
Mean Pulmonary Arterial Pressure (mPAP) ≥25 mmHg at rest on right heart catheterisation (NB: Newer ESC/ERS definition ≥20 mmHg)
🔬 Pathophysiology
Pulmonary vascular remodelling → ↑ resistance
Right ventricle under strain → hypertrophy → dilation → failure
End-stage = cor pulmonale
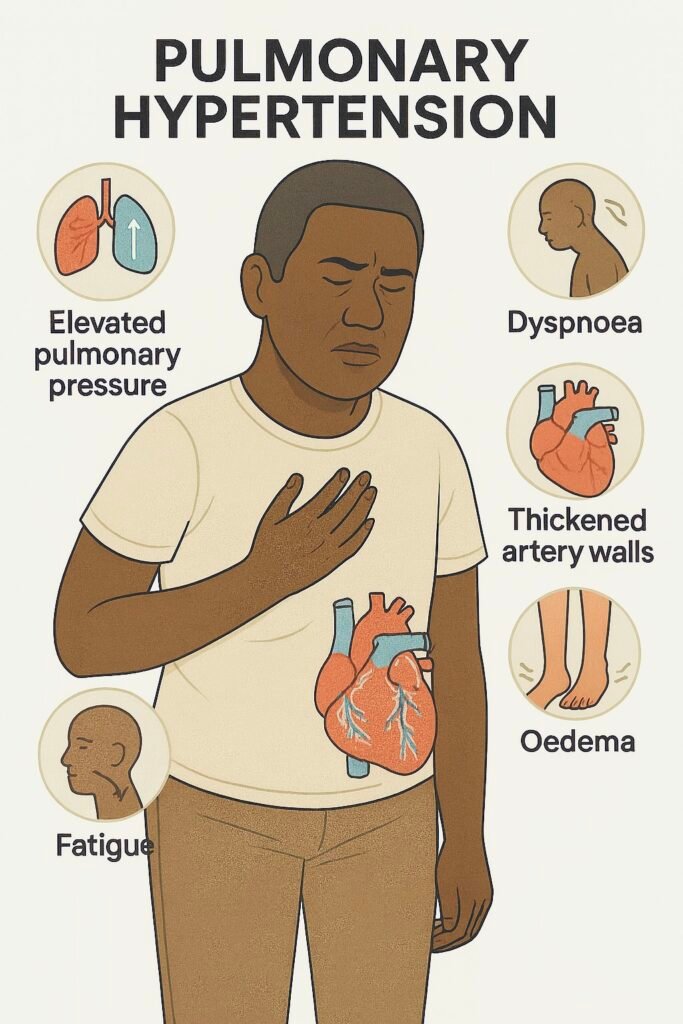
🔍 Clinical Features
Progressive dyspnoea on exertion
Fatigue, reduced exercise tolerance
Syncope on exertion (late)
Chest pain (angina-like)
Peripheral oedema, ascites
Signs: loud P2, RV heave, raised JVP, hepatomegaly, TR murmur
🛡️ Classification (WHO Groups)
| Group | Cause | Examples |
|---|---|---|
| 1 | Pulmonary arterial hypertension (PAH) | Idiopathic, CTD (scleroderma), HIV, portal HTN, drugs |
| 2 | Left heart disease | LV dysfunction, mitral/aortic valve disease |
| 3 | Chronic lung disease/hypoxia | COPD, ILD, OSA |
| 4 | Chronic thromboembolic PH (CTEPH) | Recurrent PE |
| 5 | Multifactorial/unclear | Sarcoid, haematological, metabolic |
🔬 Investigations
| Step | Investigation | Purpose |
|---|---|---|
| 1️⃣ Initial | ECG, CXR, Bloods (BNP, CTD/HIV screen) | Screen for cardiac strain, lung disease, systemic associations |
| 2️⃣ Screening | Echocardiography | Estimate pulmonary pressures, RV size/function |
| 3️⃣ Confirmatory (Gold standard) | Right heart catheterisation | mPAP ≥25 mmHg, measure wedge pressure for classification |
| 4️⃣ Aetiology work-up | V/Q scan, CTPA/HRCT, PFTs, Sleep study | Identify cause (CTEPH, ILD, COPD, OSA) |
Management

| Step | Treatment | Notes |
|---|---|---|
| General | O₂, exercise rehab, vaccines (flu/pneumo) | All groups |
| Anticoagulation | If CTEPH or idiopathic PAH | Lifelong in CTEPH |
| Diuretics | For right HF / volume overload | Symptomatic |
| Group 1 (PAH) | Endothelin antagonists (bosentan), PDE-5 inhibitors (sildenafil), prostacyclin analogues | Specialist centres |
| Group 2 | Treat underlying LV/valve disease | Eg. HF therapy, valve repair |
| Group 3 | Optimise COPD/ILD, O₂ therapy, CPAP (OSA) | |
| Group 4 | Pulmonary endarterectomy (curative if operable) + lifelong anticoagulation | |
| Group 5 | Manage underlying cause | Eg. sarcoid, haematology |
⚠️ Complications
Right heart failure (cor pulmonale)
Syncope/sudden death
Arrhythmias
Progressive exercise intolerance
CTEPH
🧐Differential Diagnoses
Heart failure
COPD/asthma
Anaemia
Interstitial lung disease
PE
Deconditioning
📌 PARA Revision Tips
Echo first → confirm with RHC (gold standard)
Group classification is high-yield
V/Q scan = best for Chronic thromboembolic pulmonary hypertension (CTEPH) (not CTPA)
Sildenafil & bosentan are exam-favourite PAH treatments
Differentiate Group 1 (normal PCWP) vs Group 2 (raised PCWP)
📆 Follow-Up & Safety Netting
Regular monitoring at PH centre
Manage contributing comorbidities
Annual echo, 6-minute walk test, BNP
Escalate rapidly if symptoms worsen
🔎 Key PARA Exam Traps
💡 Always confirm PH with RHC before PAH therapy
💡 pHTN ≠ portal HTN – common MCQ distractor
💡 If echo suggests PH, don’t start drugs before invasive confirmation
💡 V/Q > CTPA for chronic thromboembolic disease
Last updated in line with NICE NG158 – Pulmonary hypertension in adults
Published: March 2021 • Last updated: June 2022
- PARA-aligned, reviewed February 2026
PASSMAP ensures all content is NICE-aligned and reviewed for Physician Associate Registration Assessment (PARA) success.
